Authors: Lea Blasey, Wiebke Hell, Niklas Hoppe
Last updated: October 2nd 2023
1 Definition and Relevance
The healthcare sector encompasses a wide range of services and activities related to the maintenance, improvement, and restoration of human health. Included are medical facilities, healthcare professionals, pharmaceutical companies, medical technology developers, research institutions and various supporting organizations. For sufficient understanding the sector can be broadly categorized into the following five categories:
Healthcare services: These include organizations and the professionals directly involved in providing medical care and services such as hospitals, clinics, nursing homes as well as mental health and rehabilitation centres. It also includes primary, specialty and emergency care.1Akbal, H., Doğan, N.Ö. Handbook of Research on Quality and Copmetitiveness in the Healthcare Services Sector. Chapter: Lean and Smart Supply Chain Management in Healthcare. Doi: 10.4018/978-1-6684-8103-5.ch002
(2023)
The pharmaceutical industry: This industry includes the research, development, production and distribution of pharmaceutical drugs and medications and the according companies and manufacturers.2Dailey, J. W. (2023, July 21). Encyclopaedia Britannica. Pharmaceutical industry. https://www.britannica.com/technology/pharmaceutical-industry (2023)
Medical devices and equipment: This category comprises companies involved in the manufacturing, distribution and sale of medical devices, equipment and supplies such as surgical instruments, diagnostic equipment (e.g. MRI and CT scanners), patient monitoring devices, prosthetics et cetera.3Aronson, J. K., Heneghan, C., & Ferner, R. E. Medical Devices: Definition, Classification, and Regulatory Implications. Drug safety, 43(2), 83–93. Doi: 10.1007/s40264-019-00878-3 (2020)
Healthcare insurance: Health insurance companies or providers play a crucial role in the healthcare sector as they offer insurance coverage plans, which help cover the costs of medical treatments, hospital stays, medications, and other healthcare services as to provide financial protection against healthcare expenses that could expand unexpectedly and sometimes uncoverable.4Institute of Medicine (US) Committee on the Consequences of Uninsurance. Coverage Matters: Insurance and Health Care. Washington (DC): National Academies Press (US); 1, Why Health Insurance Matters. Available: https://www.ncbi.nlm.nih.gov/books/NBK223643/ (2001)
Public health and health education: This area focuses on preventive measures, health promotion, and public health initiatives. It includes government health agencies, NGOs, and educational institutions involved in public health research, disease prevention, health education, vaccination programs and so on. These entities work to improve population health and raise the very important awareness about health issues.5Nutbeam, D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health promotion international, 15(3), 259-267. (2000)
Keeping these five categories in consideration, the relevance of sustainability in the healthcare sector should be brought into perspective.
The relevance of sustainability pertains to the integration of environmentally conscious practices, social equity, and economic viability to ensure that healthcare systems can meet current and future health needs without compromising the well-being of future generations.6Marimuthu, M., & Paulose, H. Emergence of sustainability based approaches in healthcare: expanding research and practice. Procedia-Social and Behavioral Sciences, 224, 554-561. (2016) We are aware of a significant interaction between the health sector and climate change where they have been contributing and having impacts on one another. As stated in the UN CCC COP27, healthcare systems account for over 4% of global CO2 emissions, which leads us directly to the relevance of this sector in terms of sustainability.7MOOSMANN et. al., The COP27 Climate Change Conference: status of climate negotiations and issues at stake. Available at: https://www.europarl.europa.eu/RegData/etudes/STUD/2022/733989/IPOL_STU(2022)733989_EN.pdf The healthcare sector has a substantial environmental impact due to its energy consumption, waste generation, and use of natural resources. Hospitals, clinics, and other healthcare facilities contribute to greenhouse gas emissions through energy-intensive operations, transportation, and waste disposal. Addressing these issues is crucial for mitigating climate change and reducing the sector’s ecological footprint.8Brown, H. et. Al. The Energy Burden and Environmental Impact of Health Services. Am J Public Health. 2012 December; 102(12): e76–e82. doi: 10.2105/AJPH.2012.300776. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3519304/ (2012) Climate change poses various risks to public health, including increased heat-related illnesses, respiratory problems from air pollution, the spread of vector-borne diseases, and food and waterborne diseases-9Bratu, A., et. Al. The 2021 Western North American heat dome increased climate change anxiety among British Columbians: Results from a natural experiment. The Journal of Climate Change and Health, 6, 100116. (2022) The healthcare sector plays a vital role in understanding and managing these health risks, as well as educating the public and providing necessary healthcare services. Climate change impacts, such as extreme weather events and the spread of infectious diseases, can strain healthcare systems. The sector needs to enhance its resilience and adapt to changing conditions, ensuring the continuity of care and emergency response capabilities. This involves developing robust infrastructure, disaster preparedness plans, and incorporating climate change considerations into healthcare policies and practices.10Lugten, E., Hariharan, N. Strengthening Health Systems for Climate Adaption and Health Security: Key Considerations for Policy and Programming. Health Secur. September/October 2022; 20(5): 435–439. doi: 10.1089/hs.2022.0050. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9595646/ (2022) Healthcare facilities can adopt sustainable practices to reduce their environmental footprint. This includes implementing measures which will be elaborated on in the Chapter of Practical Implementation. These measures not only help mitigate climate change but also reduce costs and improve resource efficiency.11Hernández, A.-C. Reducing Healthcare´s Climate Footprint: Opportunities for European Hospitals & Health Systems. Available at: https://noharm-europe.org/sites/default/files/documents-files/4746/HCWHEurope_Climate_Report_Dec2016.pdf (2016) Research and Innovation is another way for the healthcare sector to contribute to climate change mitigation. This involves developing environmentally friendly medical technologies, exploring alternative treatment methods with lower environmental impacts, and conducting studies to better understand the health effects of climate change. Additionally, healthcare providers can promote lifestyle changes that support sustainability, such as advocating for healthier diets and active transportation. Healthcare professionals and organizations have a unique platform to advocate for climate action and sustainability. As professionals they can raise awareness about the health impacts of climate change, promote environmentally responsible policies and practices, and collaborate with other sectors to drive systemic change. By taking a leadership role, the healthcare sector can influence public opinion, policy decisions, and the implementation of sustainable practices across industries.
As climate change has negative impacts on the human health, there are significant co-benefits in mitigating and adapting the healthcare sector to it that will benefit both humans and the supporting health systems.12Jamieson, M., Wicks, A., & Boulding, T. Becoming environmentally sustainable in healthcare: an overview. Australian health review: a publication of the Australian Hospital Association, 39(4), 417–424. https://doi.org/10.1071/AH14086 (2015) By addressing these aspects, the sector can contribute to a more sustainable and resilient future.
2 Background
This chapter provides an overview of the impact of the healthcare sector on environmental and social sustainability. Within this context, indicators and measurement methods are discussed, as this will be the foundation to be able to implement sustainability strategies and measure the success of those strategies subsequently.
Environmental Impact
For the assessment of the environmental impact, it is important to look at indicators such as GHG emissions, energy consumption, resource use, and disposal of waste products, since all of these indicators have an influence on climate change, which has proven to be a fundamental threat to humanity and thus, to endanger the secure livelihood of current and future generations.13McMichael, Anthony J. Globalization, Climate Change, and Human Health. The New England journal of medicine 368, 1335–1343 (2013)
As explained in the previous chapter, the healthcare sector consists of very different types of facilities, which in turn have very different environmental impacts. For instance, for a common hospital, the following processes need to be considered: Electricity use, heat consumption, catering, electronics and large medical equipment, building infrastructure, pharmaceuticals use, laundry and water use, textiles consumption, medical and housekeeping products consumption, printing and paper use, waste and wastewater treatment.14Keller et. al. From bandages to buildings: Identifying the environmental hotspots of hospitals. Journal of Cleaner Production 319, 2-12 (2021) All of these operations need resources and produce waste materials that are released into the environment.
A study that analyzed 33 Swiss hospitals regarding the aforementioned areas of impacts came to the conclusion that “the biggest reduction in the environmental footprint of hospitals can be achieved if hospitals are energy efficient, housed in green buildings using renewable energy with management committed to reducing unnecessary operations, providing more plant-based catering services, and implementing optimized systems that reduce unnecessary pharmaceutical losses and food waste.”14Keller et. al. From bandages to buildings: Identifying the environmental hotspots of hospitals. Journal of Cleaner Production 319, 2-12 (2021)
While a hospital represents a very complex facility, most of these conclusions can be transferred to different kinds of healthcare facilities that provide stationary care for their patients.
The emphasis for pharmaceutical production firms or insurance firms differs from this analysis. For insurance firms, sustainable finance and investment is of higher importance, while for production firms, sustainable supply chain management might have more leverage to create a more sustainable healthcare system.
Despite the differences, this chapter provides an overview of indicators and measurement methods that are relevant for all types of facilities, even though the individual emphasis varies.
Evaluations of GHG emissions of the sector reveal that it is a major contributor, especially because of the carbon intensive supply chain of the wide range of pharmaceuticals, medical products and machinery. Generally, healthcare contributes to GHG emissions through energy consumption, production, transport, usage and disposal. Overall, this makes the sector account for 4.4% of net CO² emissions globally (2019).15Health Care Without Harm in collaboration with Arup. Health Care’s Climate Footprint (2019) The most important indicator that provides a comparable outcome would be to measure emissions in tons of CO² equivalents per year.
Waste disposal in the healthcare sector is an extremely important issue to address when evaluating the environmental impact, because of a few sector-specific characteristics. For hygienic reasons, a lot of one-way products are used, which results in tremendous amounts of waste. As the re-use can lead to transmission of infectious bacteria, reducing sterile one-way products represents a challenge in the sector. Apart from this, chemicals and hazardous waste also need to be taken into account, since the disposal of certain pharmaceuticals and their residues can lead to health issues like antibiotic resistance.16Walia et. al. Quantitation of antibiotic resistance genes pollution in hospital waste water effluent and Urban Clinton River Water, Michigan, USA. Current Medicine Research and Practice 6, 149–151 (2016)
An indicator to look at in order to assess and compare the environmental impact are the amounts of waste in weight (tons or kg per year), as well as shares of e.g. recycled; toxic; or non-reusable waste.
A current study estimates that high-income countries produce up to almost 11 kg of waste per hospital bed per day (kg/bed/day), while in low-income countries the production rate ranges up to 6 kg. According to the study, 85% of the total [WH1] amount of waste generated as a result of healthcare activities is non-hazardous. The remaining 15% are hazardous materials which are infectious, radioactive or toxic. In low-income countries, problems arise due to unseparated hazardous and non-hazardous waste.17Janik-Karpinska et. al. Healthcare Waste – A Serious Problem for Global Health. Healthcare (Basel, Switzerland) 11, 242 (2023)
To measure the energy efficiency of healthcare facilities, one needs to look at the overall energy consumption in MWh or GJ per year, as well as shares of renewable energy.
A study that analyzed sources of emissions split by production sectors in the global healthcare industry implies that the generation and distribution of electricity, gas and heating or cooling contributes the most to the sector’s emissions with 40%.15Health Care Without Harm in collaboration with Arup. Health Care’s Climate Footprint (2019) Thus, independent from the type of facility, energy use seems to be a major contributor to emissions and environmental damage.
Due to rising drinking water scarcity,18Pankaj C. et.al. Role of Industries in Water Scarcity and Its Adverse Effects on Environment and Human Health in Environmental Concerns and Sustainable Development (eds. Shukla, V; Kumar, N.) 235-256 (Springer, 2020) water use is a highly relevant indicator for the impact of the sector on sustainability. It can be measured through m³ water use per year, including information about shares of drinking water compared to process water, and about shares of wastewater, since sewage segments can potentially endanger the environment, depending on the kind of disposal.
Generally, resource use is an important factor to analyze since the reduction of material use is a preventive environmental protection measure. Non-renewable raw materials such as fossil fuels used for plastic production should be avoided or reduced, since plastics have been estimated to account for 30% of all healthcare waste.19McGain et. al. An audit of intensive care unit recyclable waste. Anaesthesia 64, 1299–1302 (2009) Renewable resources should be used while respecting assimilative capacities of the environment to ensure resource provision for future generations.20Kanning, H. Managementregeln der Nachhaltigkeit in Betriebliches Nachhaltigkeitsmanagement (eds. Baumast; Pape) 33-34 (UTB; Verlag Eugen Ulmer 2022) Additionally, reducing resource use goes hand in hand with the reduction of waste materials. To compare and find the most efficient strategies to reduce the use of resources, material efficiency can be measured in tons of certain materials and substances per year. For a truthful analysis, the supply chain of medical products must be sufficiently transparent. Apart from plastics, chemicals and pharmaceuticals, healthcare facilities with stationary care also need to include the nutrition they provide to their assessment.
Furthermore, within the frame of environmental sustainability, the impact of the sector on biodiversity should be included. Due to the complexity of ecosystems and their living organisms, this is hard to grasp and all factors mentioned above influence biodiversity directly or indirectly. Nonetheless, reporting standard initiatives like EMAS suggest m² land-use as one of the core indicators.21Bodensee-Stiftung and Global Nature Fund. Leitfaden 2023 – Schutz der biologischen Vielfalt im Rahmen von Umweltmanagementsystemen (2023) Here, apart from healthcare facilities themselves, the supply chain and production facilities play a fundamental role.
Social Impact
The analysis of the social impact is more complex, since it is mostly impossible to fully reflect the impact in quantitative data and standardized methods. Different cultures, preferences, values and norms need to be taken into account, as social indicators may have different implications in different regions and contexts.
Literature on the social dimension of sustainability suggests concepts such as well-being, equity, human rights and diversity as guiding principles.22Magis, K.; Shinn, C. Emerging Principles of Social Sustainability in Understanding the Social Dimension of Sustainability (eds. Dillard et. al.) 15-44 (Routledge, 2009) Some measurable indicators like life expectancy, education and income may provide some orientation regarding the social impact. Nevertheless, without additional information about the context, these measurable indicators may result in misleading conclusions and biased outcomes.
Many sustainability reporting norms like the Global Reporting Initiative (GRI) suggest to follow the UN sustainable development goals23Department of Economic and Social Affairs, Sustainable Development. The 17 SDGs. United Nations. https://sdgs.un.org/goals (2023) as guiding principles and to focus on the ones that are most relevant to the industry or sector of concern.
Generally, healthcare itself is considered a social service, as it represents an infrastructure that is meant to provide “Good health and well-being” (SDG 3). Nonetheless, the implementation and maintenance of a healthcare system is connected to several social challenges. SDGs 10 “Reduced Inequalities” and 16 “Peace, Justice and Strong Institutions” are especially relevant when it comes to discrimination in healthcare. Inequalities can be reduced by ensuring to provide the best possible medical care to each individual, regardless of their “race/ethnicity, gender, sexual orientation, immigration status, physical disability status, and socioeconomic level”.24Stanford; Fatima. The Importance of Diversity and Inclusion in the Healthcare Workforce. Journal of the National Medical Association 112, 247–249 (2020)
Depending on the healthcare system of a country or region, privileges are another reason of discrimination, since the scarcity of medical resources or human resources like doctors and nurses will lead to patient prioritization. This represents a social dilemma, as a choice needs to be made, but the fairness of that choice depends on the system that is in place and the moral compass that the person in charge of the decision is following.25Deshpande, Satish P. A Study of Ethical Decision Making by Physicians and Nurses in Hospitals. Journal of Business Ethics 90, 387–397 (2009) Generally, one could measure the efficiency and success of a medical institution in the number of patients saved from a certain disease or in death rates, but to look at the whole picture, the quality of life and well-being of surviving patients need to be considered as well, which makes the data collection for such indicators much more complex.
Discrimination can also occur within the frame of employment. Gender equality (SDG 5) is a goal that can be measured and quantified in the ratio in male, female and diverse employees in a healthcare facility.
While women represent 71% of the global healthcare personnel, they remain underrepresented in healthcare leadership, relative to the proportion in the workforce.23Mousa et. al. Advancing women in healthcare leadership: A systematic review and meta-synthesis of multi-sector evidence on organisational interventions. EClinicalMedicine 39, 101084 (2021) Thus, it is important to subdivide indicators like gender-based employment ratios into jobs and responsibilities of the employees to provide transparent information. Although ratios provide a straightforward comparable indicator, behavioral data and surveys may help to capture trends in what kind of barriers to gender equality are especially relevant within an institution. The following potential barriers for women to achieve leadership roles in the healthcare sector have been identified by recent studies: “[…] reduced capacity due to career disruption and external responsibilities; credibility assumptions around women in leadership and perceived capability and confidence”.23Mousa et. al. Advancing women in healthcare leadership: A systematic review and meta-synthesis of multi-sector evidence on organisational interventions. EClinicalMedicine 39, 101084 (2021)
When talking about gender equality, inclusive thinking to create an LGBTQIA+ friendly environment both within the workforce and for patients is highly important in the healthcare sector. Surveys on transgender people have shown that they encounter interpersonal and structural barriers, which lead to avoidance of healthcare due to anticipated discrimination,26Kcomt L. et. al. Healthcare avoidance due to anticipated discrimination among transgender people: A call to create trans-affirmative environments. SSM – population health 11, 100608 (2020) which in turn negatively affects their health and well-being.
Apart from this, healthcare facility managers bear a lot of responsibility towards their employees, since it is their duty to ensure a safe working environment and supply the measures to protect their staff from exposure to diseases and other health threats within the working environment.
To provide a safe working environment in a healthcare facility means protecting the employees’ mental health and job satisfaction, which can be affected by factors like shift work and extended work hours, safety climate and culture, teamwork, and communication. Furthermore, it means physical protection from chemical hazards (e.g., waste anesthetics, hazardous drugs, cleaning compounds) and airborne and bloodborne pathogen exposure.27Geiger-Brown, J.; Lipscomb, J. The Health Care Work Environment and Adverse Health and Safety Consequences for Nurses. Annual review of nursing research 28, 191–231 (2010) Especially in healthcare, providing a safe working environment for employees is directly intertwined with the patients’ safety. A work environment that facilitates patient-centered care has proven to increase job satisfaction among nurses and in thus to avoid medical errors.28Rathert, C.; May, D. R. Health care work environments, employee satisfaction, and patient safety. Health Care Management Review 32, 2-11 (2007)
Providing a safe work environment can be categorized under SDG 8 “Decent work and economic growth”, which also includes fair salaries and to avoid discrimination in the form of pay gaps. Studies implied that using weighted global estimates, the gender pay gap in the health and care sector ranges from about 15% to about 24%.29The International Labor Organization and the World Health Organization. The gender pay gap in the health and care sector (2022)
Concerning this matter, the social and economic dimensions of the impact on sustainability of the healthcare sector are closely interlinked.
Principally, the economic impact of the healthcare sector varies among countries and regions. In most countries, it is a major employment provider and economic driver, e.g., in the USA30KFF. Health Care Employment as a Percent of Total Employment https://www.kff.org/other/state-indicator/health-care-employment-as-total (2022) and Germany31Bundesgesundheitsministerium. Personal in der Gesundheitswirtschaft https://www.bundesgesundheitsministerium.de/fileadmin/Dateien/2_Bilder/2_Grafiken/Infografiken/Gesundheit/Infografik_Gesundheitspersonal.pdf (2023) , the sector makes up more than 12% of jobs out of total employment.
Operations at healthcare facilities are deeply interlinked with production industries for pharmaceuticals and medical devices, and the regional economic impact these industries provide. Laws and regulations have a major influence, as they may incentivize e.g., to make profit-oriented decisions, which can stand in the way of ethical decision making. This occurs particularly in cases of divergence between private profit-oriented interests and public health needs.32Heled et. al. The problem with relying on profit-driven models to produce pandemic drugs. Journal of law and the biosciences 7, 1–23 (2023)
“Industry, innovation and infrastructure” (SDG 9) must be considered when examining the economic impact of the sector, since innovations and technology are important to increase cost- and time efficiency with the aim to provide better healthcare. However, when comparing a country’s spending, prices and general conditions need to be taken into account. High investments in healthcare do not necessarily lead to a better functioning health system.33Preeti Vankar. Health expenditure as a percentage of gross domestic product (GDP) in selected countries in 2022. Statista https://www.statista.com/statistics/268826/health-expenditure-as-gdp-percentage-in-oecd-countries/ (2022)
Regarding cost efficiency, it is worth mentioning that environmental protection measures have proven to reduce costs,34International Standards Organization. ISO 14001 Environmental Management Systems (2015) for instance through energy efficiency, risk management, and reduction of resource use.
Furthermore, within the economic scope, healthcare facilities are responsible for sustainable controlling, as well as sustainable finance and investment options, just like every other industry. The latter is especially relevant for insurance firms.
An understanding of the economic impact of the sector is essential. However, when it comes to sustainability measures and the practical implementation of those, this article sets its focus on the environmental dimension.
3 Practical Implementation
This chapter delves into the practical implementation of sustainability measures within hospitals and similar patient-focused facilities. As the stewards of well-being, these institutions must bridge the gap between patient care and environmental responsibility, addressing pressing environmental challenges while fostering resilient healthcare systems.
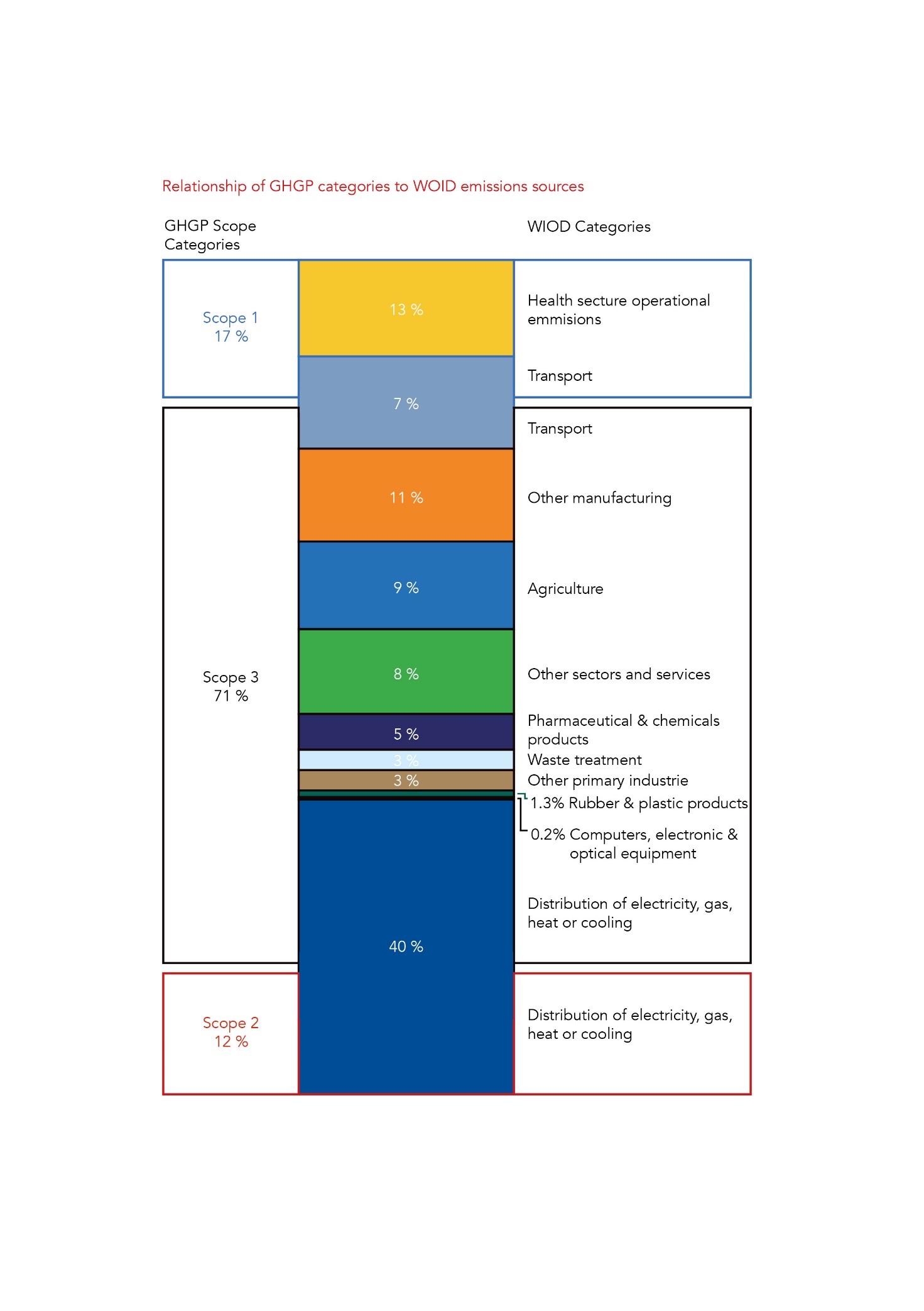
| Figure 1: Relationship of GHGP(Greenhouse Gas Protocol) categories to WIOD(World Input Output Da-tabase) emissions sources35Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health 57, p.1768 (2021) |
To comprehend and categorize diverse approaches to sustainability implementation, it is important to understand the distribution of healthcare facilities’ emissions. Emissions within healthcare are categorized into the three scopes pictured in Figure 1. Scope 1 (17% of total) encompasses direct emissions on-site, e.g. gas combustion for hot water. Scope 2 (12%) entails indirect emissions from purchased energy. The majority of healthcare’s carbon footprint (71%) stems from Scope 3 emissions: product purchasing and the healthcare supply chain. This covers medical consumables, pharmaceuticals, devices, equipment, food, agriculture, and paper (see figure 1).35Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health 57, p.1768 (2021) In addition to emissions, healthcare also generates significant quantities of waste, a consequence largely attributed to the pervasive use of single-use consumables.36Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.1 (2019) A single operation room produces the same amount of waste in a week as a family of four.35Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health 57, p.1768 (2021) By comprehending these emissions divisions and waste challenges, different tackling points for implementing sustainability can be identified. For instance, the GGHH (Global Green and Healthy Hospitals), a collaborative network of health institutions with the goal of reducing the environmental footprints and fostering a healthier future, outlines ten goals to improve healthcare’s environmental impacts (see figure 2).35Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health 57, p.1768 (2021)
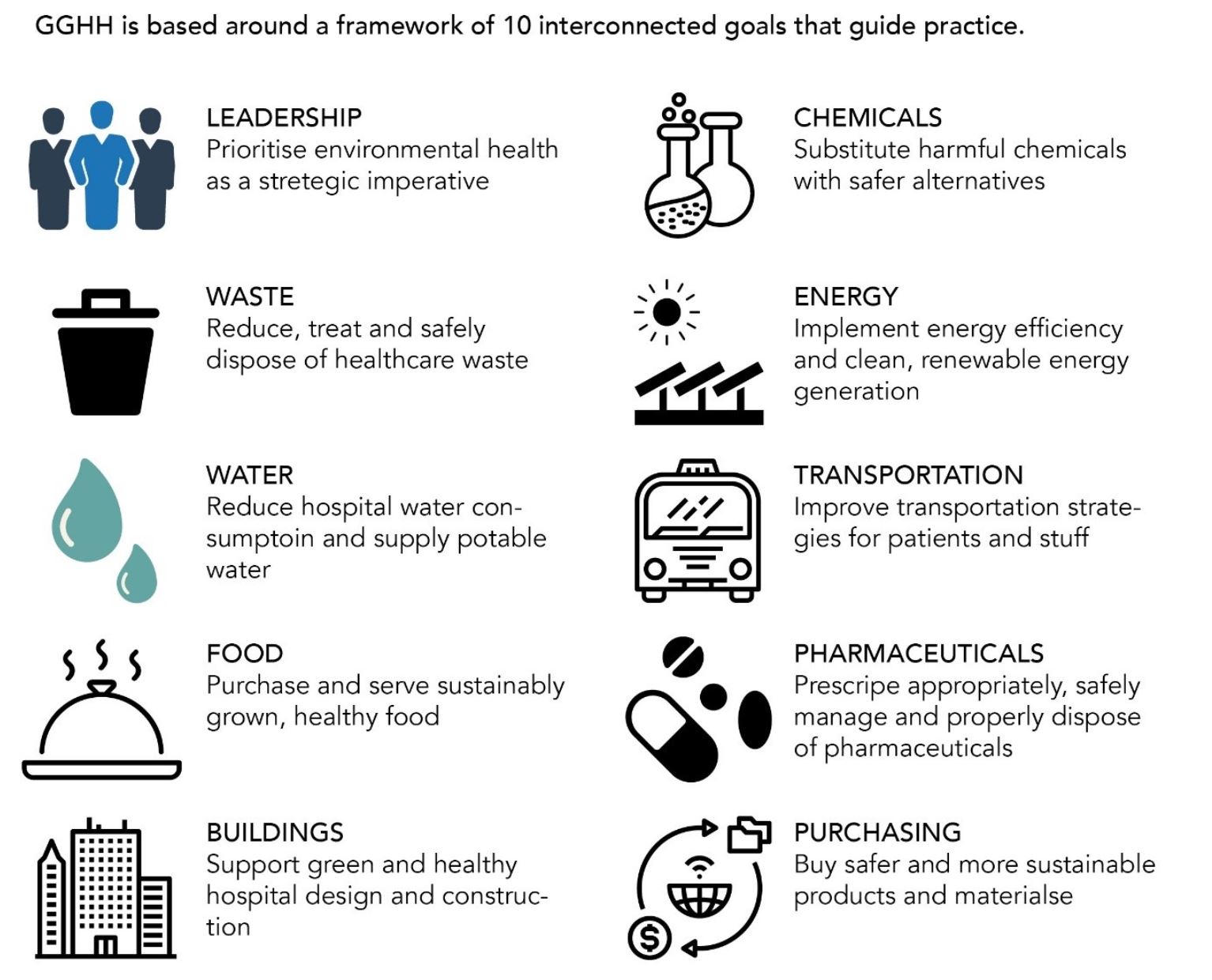
| Figure 2: The 10 Goals of the GGHH37World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.3 (2009) |
In a parallel effort, the World Health Organization, collaborating with Healthcare without Harm (HCWH), outlines seven strategies to foster a more climate-friendly healthcare sector:
- Energy Efficiency: Reduce hospital energy consumption and costs through efficiency measures
- Green Building Design: Optimize hospitals for reduced energy and resource demand
- Alternative Energy Generation: Produce clean, renewable energy onsite for reliability
- Transportation: Use alternative fuels, promote walking, cycling, and efficient site placement
- Sustainable Food: Offer local, sustainably grown food for staff and patients
- Waste Management: Reduce, reuse, recycle, avoid incineration
- Water Conservation: Conserve water, prioritize safe alternatives to bottled water 38Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.2 (2019)
Drawing from the GGHH goals and WHO strategies, distinct avenues for sustainable practices emerge, forming the basis for further discussion in the ensuing chapters.
Energy
Energy efficiency and sustainability, while not limited to a particular sector, bear particular significance within the healthcare domain. Hospitals, as life-saving hubs, maintain an unceasing demand for energy, driven by the imperative to sustain operations round-the-clock. This necessity intensifies within critical areas such as intensive care units and emergency rooms, which must remain ready at all times. The healthcare sector’s stringent requirements for cleanliness and sterilization, particularly within surgical environments, translate into elevated electrical consumption aimed at maintaining optimal conditions.39World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.10 (2009) Embedded within the standard operating procedures of most healthcare facilities, energy-intensive processes span a spectrum ranging from water heating to indoor air temperature and humidity control, illumination, ventilation, and a myriad of clinical procedures. These processes, while vital, contribute significantly to GHG emissions and the sector’s overall carbon footprint.40Health Care Without Harm and Practice Greenhealth: Adressing Climate Change in the Health Care Setting, p.6-7. (n.d.)
Energy efficiency within the healthcare sector embodies a dynamic spectrum of different strategies and initiatives. Given the complexity and uniqueness of healthcare facilities, there is no one-size-fits-all solution. Instead, a multifaceted array of approaches is required to address the distinct energy challenges presented by diverse healthcare environments. Examples of these diverse approaches include fostering energy efficiency in buildings, embracing on-site renewable energy, selecting energy-efficient products, and transitioning to renewable energy sources.39World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.10 (2009)
A good example of effective energy-saving is the Hospital General Dr Agosthino Neto in Cuba. In 2006, the hospital launched the “Integrated System for Saving and Reducing Energy,” starting with a comprehensive energy audit. The audit identified key energy sources along with 30 energy-related issues. By resolving 23 of these concerns, the hospital achieved remarkable outcomes. Upgrades such as replacing air conditioners and refrigerators with efficient models, enhancing electrical systems and boilers, and reducing fuel oil consumption, led to a commendable 21% reduction in energy use. Parallel to the technological enhancements a widespread education campaign involving staff members at all levels was realized.41Altin, A. & Altin, S.: Sustainable Water and Wastewater Management in Hospitals, in: The Turkish Journal of Occupational / Environmental Medicine and Safety 2 (1), p.2 (2007)
Water
The healthcare sector, more specific hospitals, ranks among the major consumers of water within urban landscapes. The quality and availability of water in hospitals are of vital importance, impacting patient health and daily hospital operations.42Zhu, Q., Johnson, S. & Sarkis, J.: Lean six sigma and environmental sustainability: a hospital perspective, in: Supply Chain Forum: An International Journal, p.4 (2018) The healthcare sector’s consumption of water holds significant weight within the broader context of water usage. In the United States, hospitals and healthcare facilities account for a notable portion, comprising 7% of the total water consumption within commercial and institutional establishments.43Bross, L. et. al.: Public health without water? Emergency water supply and minimum supply standards of hospitals in high-income countries using the example of Germany and Austria, in: Water Policy 23 (2), p.1 (2021) The disruption of water supply can yield far-reaching consequences that extend beyond hospital functioning to societal safety, which emphasizes the criticality of this resource.44Verlicchi, P. et. al.: Hospital effluents as a source of emerging pollutants: An overview of micropollutants and sustainable treatment options, in: Journal of Hydrology 389, p.1 (2010) Complementing water consumption, the management of hospital wastewater assumes equal significance, since hospital wastewater contains a variety of toxic or persistent substances like pharmaceutical solvents or disinfectants.45Altin, A. & Altin, S.: Sustainable Water and Wastewater Management in Hospitals, in: The Turkish Journal of Occupational / Environmental Medicine and Safety 2 (1), p.6 (2007)
Efforts to enhance water efficiency span a diverse spectrum of strategies, given the distinctiveness of healthcare settings and can in some cases be linked with an effective waste water management. For instance, wastewater generated within dialysis units, devoid of bacteria or toxins, can find purpose as greywater for toilet flushing or turf irrigation.46World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.21 (2009) Water-conserving measures encompass optimizing pump design, retrofitting water faucets, upgrading toilet and urinal flush valves, and refurbishing refrigeration systems. These measures can collectively lead to substantial reductions in water usage. For instance, Norwood Hospital in Massachusetts, USA, achieved a remarkable 29% reduction in water consumption over three years. The hospital’s implementation of a range of water conservation measures resulted in cutting water usage from 51.2 to 36.6 million gallons annually. Notably, this water-efficient approach also yielded financial benefits, with the hospital saving around US$14,000 each year.48Health Care Without Harm and Practice Greenhealth: Adressing Climate Change in the Health Care Setting, p.10. (n.d.)
Food
The role of sustainable food practices within healthcare institutions is a concise yet impactful chapter. While food might not be an obvious environmental concern for healthcare, it holds significant potential to influence both the environment and patient well-being. The modern food system, with its intensive production of single crops or animals, heavily relies on petroleum-based resources like fertilizers, pesticides, and transportation fuel. This system has become a major contributor to GHG emissions, surpassing even the transportation sector. Notably, the livestock sector alone generates around 18% of global GHG emissions, emphasizing the environmental impact of food choices. Hospitals’ influence on climate change extends to their purchasing power.48Health Care Without Harm and Practice Greenhealth: Adressing Climate Change in the Health Care Setting, p.10. (n.d.) The distance food travels, highlighted by the average 1,500 to 2,400-mile (2414 to 3862-km) journey from farm to plate, significantly contributes to energy-related emissions. Addressing this, healthcare facilities can make a substantial difference by selecting foods that minimize GHG emissions.49World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.19 (2009).
In the UK, various NHS hospitals are actively enhancing their offerings of locally sourced and organic foods by 10%, a shift that holds particular significance considering the NHS spends approximately 500 million pounds (582 million €) on food, serving 300 million meals annually. This endeavor is poised to generate a notable impact.50Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health 57, p.1771 (2021) Simultaneously, Sydney Children’s Hospitals Network (SCHN) has demonstrated a community-driven initiative by introducing farmers markets. These markets promote healthy eating and foster connections within the hospital community by providing access to fresh, local products to staff and patients and offer education through talks.48Health Care Without Harm and Practice Greenhealth: Adressing Climate Change in the Health Care Setting, p.10. (n.d.) Moreover, strategies such as decreasing meat protein on menus, opting for local and seasonal foods, incorporating organic choices when feasible, and implementing waste reduction practices, offer concrete steps that hospitals can take toward sustainability and positive impact.51EPA Carbon Pollution from Transportation https://www.epa.gov/transportation-air-pollution-and-climate-change/carbon-pollution-transportation
Transportation
The transportation sector plays a pivotal role in healthcare’s overall environmental impact. In the United States, transportation accounts for a substantial 29% of greenhouse gas emissions, making it the largest contributor. The burning of fossil fuels for vehicle propulsion releases large amounts of CO2 along with methane (CH4) and nitrous oxide (N2O)—potent GHG.52Health Care Without Harm and Practice Greenhealth: Adressing Climate Change in the Health Care Setting, p.5. (n.d.) Health care facilities rely heavily on transportation systems to move patients, workers, supplies, and waste, and so careful analysis and redesign of hospital transportation can have significant climate change mitigation benefits. Strategies for emissions reduction in the transportation sector center on reducing overall travel or adopting more emissions-efficient modes of transportation, such as higher efficiency or alternate fuel vehicles. Notably, these efforts hold the potential to curtail other vehicle emissions known to adversely impact health, including nitrogen oxides, benzene, particulate matter, volatile organic compounds, and carbon monoxide.50Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health 57, p.1771 (2021)
Healthcare institutions have demonstrated their capacity to inspire positive change within transportation practices. For instance, the Sydney Children’s Hospitals Network (SCHN) has advanced staff active transport by providing secure bike storage, offering fleet bikes for commuting, and collaborating with the local council to provide cycling skills courses.53Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health 57, p.1772 (2021) Seattle Children’s Hospital in the USA has taken an innovative approach by establishing a comprehensive employee transportation program that promotes active and public transportation, featuring an on-site bike shop and discounted public transport fares.54World Health Organization: Health in the green Economy, Health Care Facilities, p.2 (2011)
Furthermore, healthcare-specific technologies, like telemedicine, hold potential to significantly reduce emissions. Telehealth systems can not only trim the carbon footprint associated with travel but also enhance accessibility and outcomes for the vulnerable. While acknowledging the importance of direct contact between patients and healthcare providers, telemedicine holds the potential to reshape primary care and, in turn, decrease the need for hospitalization, which bears a high environmental footprint.55Hu et. al. : Sustainability in Health Care, in: Annual Review of Environment and Resources 47, p.183 (2022) The emergence of telemedicine has been significantly accelerated by the COVID-19 pandemic, resulting in a noteworthy decrease in in-person visits and the corresponding GHG emissions from transportation. A recent study illustrated a remarkable 46.2% decrease in in-person visits following a healthcare system’s adoption of telehealth, resulting in a substantial reduction of transportation-related greenhouse gas emissions.56Mehra, R. & Sharma, M. K.: Measures of Sustainability in Healthcare, in: Sustainability Analytics and Modeling 1, p.2 (2021) These advancements hint at the possibility of telemedicine improving primary care, thereby potentially reducing the need for hospitalization and the associated environmental footprint.
Design and Construction
The design and construction of healthcare facilities play a crucial role in shaping their environmental impact and long-term sustainability. The physical environment in which medical care is provided holds a significant impact on health and well-being. Integrating green design principles into facilities’ design processes can lead to breakthrough improvements compared to traditional approaches. Advocating for clean energy sources along with the efficient use of energy becomes a central focus.38Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.2 (2019)
One promising concept gaining traction within the healthcare sector is the “LEED for Healthcare” certification offered by the United States Green Building Council. This initiative focuses on setting standards and specifications for achieving leadership in energy and environmental design specifically tailored for healthcare institutions.57World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.12 (2009) By emphasizing sustainability in design and construction, healthcare facilities can significantly reduce their energy consumption and GHG emissions.
Environmental sustainability can be seamlessly integrated into healthcare facilities through the incorporation of green building principles during design and construction, as well as in retrofits of existing hospitals. Such principles encompass various aspects, ranging from strategic site selection and local building material usage, to incorporating design elements like day lighting, natural ventilation, and green roofs.57World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.12 (2009) Remarkably, this proactive approach can effectively moderate a facility’s climate footprint even before being put into operation.
Real-world examples underscore the transformative potential of sustainable design practices. At Changi General Hospital in Singapore, a range of innovative features such as hydroponic gardens, sun-shading devices, and motion sensor lighting contribute to substantial energy and water savings.57World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.12 (2009) Similarly, Meyer Children’s Hospital in Italy demonstrates a commitment to creating a healing environment through design elements like high ceilings, landscaped roofs, and energy-efficient ventilation systems.58Langstaff, K. & Brzozowski, V.: Managing environmental sustainability in a healthcare setting, in: Healthcare Management Forum 30(2), p. 86 (2017) Another notable example is St. Joseph’s Healthcare Hamilton (SJHH), whose West 5th facility achieved LEED gold certification through a combination of design choices. These choices included preserving mature trees, minimizing solar heat gain, utilizing low-emitting materials, optimizing water consumption, and diverting construction waste through recycling plans.59Health Care Without Harm and Practice Greenhealth: Adressing Climate Change in the Health Care Setting, p.8. (n.d.) These instances affirm the possibility of harmonizing healthcare needs with eco-friendly design choices.
Sustainable design goes beyond resource management to encompass responsible land use and material selection. Siting healthcare facilities near public transportation routes, utilizing locally sourced building materials, and practicing integrated land use and development planning are all strategies that contribute to reducing energy consumption and GHG emissions.60Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health 57, p.1767 (2021) Notably, these practices also mitigate the ecological disruption caused by raw material extraction, thereby protecting natural carbon sinks and reducing fossil fuel energy requirements for material production and transport.
Supply Chain and Procurement
The supply chain and procurement processes within healthcare play a pivotal role in shaping both the environmental footprint and the economic landscape of the sector. As the healthcare industry continues to grow, its impact on sustainability becomes increasingly evident. Considerable attention has been drawn to the environmental implications of pharmaceuticals, a significant contributor to the carbon footprint of healthcare systems worldwide. In the UK’s National Health Service (NHS), for instance, a comprehensive carbon audit revealed that pharmaceuticals alone were responsible for 25% of total emissions, with specific medications like anesthetic gases and metered-dose inhalers exerting disproportionate influence.61Mehra, R. & Sharma, M. K.: Measures of Sustainability in Healthcare, in: Sustainability Analytics and Modeling 1, p.1 (2021) This revelation underscores the need for careful scrutiny and optimization of procurement practices.
Health expenditure constitutes a substantial portion of global economic output, accounting for around 10%, while the scope of healthcare procurement extends beyond medical supplies to encompass a diverse range of goods and services.39World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.10 (2009) The healthcare sector’s economic leverage can be harnessed to promote sustainable procurement practices, where environmentally friendly products are prioritized. This approach aligns with the “shopping green” concept, encouraging healthcare institutions to procure materials and products with minimal carbon impact, such as energy-efficient equipment, locally sourced goods, and low-energy lighting fixtures.62Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.1-2 (2019)
Environmental considerations extend to the entire lifecycle of medical products. The concept of Environmentally Preferred Purchasing (EPP) has gained traction as a strategic approach for healthcare institutions to make sustainable procurement decisions. EPP programs guide the selection of products that align with public health safety while taking into account the environmental impact of raw materials, manufacturing processes, and disposal solutions.63Zhu, Q., Johnson, S. & Sarkis, J.: Lean six sigma and environmental sustainability: a hospital perspective, in: Supply Chain Forum: An International Journal, p.3 (2018) This holistic approach ensures that healthcare institutions contribute positively to both patient care and environmental preservation.
The healthcare supply chain’s complexity stems from its direct impact on patient care and community health systems, differentiating it from many other industries.55Hu et. al. : Sustainability in Health Care, in: Annual Review of Environment and Resources 47, p.183 (2022) Moreover, the healthcare sector’s reliance on supply chains, which contributes significantly to GHG emissions, necessitates innovative solutions. Frameworks like the Environmental Product Declaration (ISO 14025) offer a means to quantify and report the carbon footprint of medical products, potentially prompting suppliers to develop more sustainable offerings.54World Health Organization: Health in the green Economy, Health Care Facilities, p.2 (2011) In the case of England’s NHS, efficient procurement management was estimated to represent 60% of the carbon footprint, with a reduction of pharmaceutical procurement predicted to lead to a proportional reduction in carbon emissions.64Langstaff, K. & Brzozowski, V.: Managing environmental sustainability in a healthcare setting, in: Healthcare Management Forum 30(2), p. 84 (2017) This underscores the significance of supply chain management not only in terms of economic efficiency but also in mitigating environmental impacts.
A practical illustration of sustainable procurement can be found in the initiatives undertaken by St. Joseph’s Healthcare Hamilton (SJHH). Collaborating with procurement partners, SJHH embarked on the development of a standardized scorecard designed to guide the evaluation of products, equipment, and services. This innovative approach equips procurement managers with a comprehensive tool to assess whether the items under consideration align with stringent environmental criteria.36Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.1 (2019) By integrating environmental considerations into the procurement process, SJHH not only emphasizes their commitment to sustainability but also ensures that the products and services chosen contribute positively to the institution’s ecological goals.
Waste
Healthcare facilities’ waste generation and medical equipment management significantly impact both environmental sustainability and operational efficiency within the sector. With American healthcare establishments discarding over four billion pounds (1.8 billion kgs) of medical waste annually, healthcare ranks as the second-largest contributor to US landfill waste after the food industry.65Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.4 (2019) This waste includes both general and hazardous types, and improper handling of the latter poses serious threats due to chemicals and pathogens contaminating soil, water, and air, endangering communities.36Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.1 (2019)
Several different initiatives and organizations emerged to tackle the severe issue of waste output. Established in 1998, Practice Green Health is a leading force in promoting sustainability across the healthcare sector. With over 1400 partners representing 7500 global healthcare facilities, including hospitals and clinics, Practice Green Health actively engages in waste management and reduction initiatives, resulting in substantial waste reduction—an average of 338 tons annually.66Hu et. al. : Sustainability in Health Care, in: Annual Review of Environment and Resources 47, p.180 (2022) Central to waste management in healthcare is addressing the environmental impact of single-use plastics, which are pervasive in the sector. Transitioning from conventional plastics to bio-based alternatives offers a tangible pathway to reduce the ecological footprint of healthcare services.38Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.2 (2019) Also the adoption of circular economy principles presents a comprehensive framework to assess and manage material impacts throughout their lifecycle. By embracing circular economy(wiki link) principles, healthcare institutions can identify opportunities for product longevity, reuse, recycling, and responsible disposal.
In tackling the complex challenge of waste reduction, the “Five Rs” principles – reduce, reuse, recycle, re-think, and research – emerge as practical and actionable solutions.38Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.2 (2019) These principles collectively advocate for a holistic waste management approach. To “reduce,” healthcare facilities can strategically isolate waste categories, optimize packaging, and minimize waste production.67 Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.3 (2019) The principle of “reuse” promotes repurposing medical equipment, leading to significant waste diversion while upholding safety standards.67Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.3 (2019) Likewise, “recycling” facilitates the recovery of valuable materials and devices that might otherwise contribute to landfill waste.65Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.4 (2019) The principles of “re-think” and “research” encourage healthcare institutions to challenge traditional practices and explore innovative solutions. For instance, the conventional disposal of biohazardous waste through incineration, while reducing volume and neutralizing toxicity, results in detrimental emissions. These consequences can be addressed through rethinking and researching alternative disposal methods.68Health Care Without Harm and Practice Greenhealth: Adressing Climate Change in the Health Care Setting, p.9. (n.d.)
Practical examples illustrate the transformative impact of these principles. The Children’s Hospital of Eastern Ontario’s partnership with Blue-Zone Ltd. exemplifies the ‘rethink’ and ‘research’ principles in action, extending the lifecycle of anesthetic gases by ten to twenty times and reducing emissions as well as costs, through an innovative anesthetic gas capture technology.67Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.3 (2019) The ‘recycle’ principle comes alive through initiatives like the Engineering World Health Foundation, that refurbishes and donates medical equipment to less fortunate countries. In essence, discarded medical devices that would otherwise contribute to landfill waste, find a renewed purpose through recycling and refurbishing efforts, simultaneously addressing the issue of waste and improving healthcare access for underserved communities.69European Commission. Website:https://climate.ec.europa.eu/climate-change/consequences-climate-change_en (2023) These instances underscore the potential of sustainable waste management, driving equitable healthcare solutions while minimizing environmental impact.
4 Drivers and Barriers
4.1 Drivers
To comprehend the sector specific motivation for sustainability in healthcare, there are different drivers worth mentioning. Sustainability in healthcare is driven by a combination of factors that emphasize the need to balance economic, environmental, and social considerations to ensure the long-term viability and positive impact of healthcare systems. A driver to mention is the environmental concern of global climate change, which is a significant threat not only to human health but also planet health. Some health effects from climate change are projected to include changes in the impact and distribution of diseases. Just like the coronavirus, other viruses, diseases and plant pests are projected to evolve with the ongoing change in climate. A change in air quality and ozone is also projected to pose risks.70Government of the Netherlands. Sustainable Healthcare. Website: https://www.government.nl/topics/sustainable-healthcare/more-sustainability-in-the-care-sector#:~:text=The%203rd%20Green%20Deal%20on,on%20climate%20and%20the%20environment. (2023) Growing awareness of environmental challenges, resource scarcity, and pollution has led healthcare organizations to adopt more sustainable practices. Sustainable healthcare as stated in the third European Green Deal aims to achieve a shift towards green, climate-neutral healthcare, emphasize prevention and focus more on factors that enhance people’s health and reduce the sector´s negative effects on climate and the environment.71WHO guidance for climate-resilient and environmentally sustainable health care facilities. Geneva: World Health Organization; Licence: CC BY-NC-SA 3.0 IGO. (2020) Governments and international organizations are also implementing regulations and policies that encourage healthcare organizations to adopt sustainable practices. These regulations often include requirements for waste management, energy efficiency, and reduction of harmful emissions. To name one example of frameworks, in 2020 the World Health Organization published a report on guidance for climate-resilient and environmentally sustainable health care facilities.72Sherman, J. et.al. The Green Print: Advancement of Environmental Sustainability in Healthcare, Resources, Conservation and Recycling, Volume 161, 104882, ISSN 0921-3449, Doi: 10.1016/j.resconrec.2020.104882. (2020) From an economic approach, implementing sustainable practices can lead to long-term cost saving. Energy-efficient buildings, waste reduction strategies, water conservation methods and optimized resource use can help healthcare facilities operate more efficiently.73Arab ul Mateen, Qasim Ali Nisar, Nadia Nasir, Fostering pro-environmental behaviors in the healthcare organizations: An empirical analysis of psychological and strategic factors, Asia Pacific Management Review, Volume 28, Issue 1, Pages 13-23, ISSN 1029-3132, Doi: 10.1016/j.apmrv.2022.01.004., (2023) Patients and the public are becoming more conscious of the environmental and social impacts of healthcare services. There is an increasing demand for healthcare providers to demonstrate their commitment to sustainability, which can influence organizations to adopt greener practices.74Kruk, M. E., et. al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. The Lancet. Global health, 6(11), e1196–e1252. Doi: 10.1016/S2214-109X(18)30386-3(2018) Sustainable practices can lead to improved patient outcomes, for example, efficient waste management reduces the risk of infections, and promoting healthy behavior can prevent chronic diseases.75Tomaselli, G., Garg, L., Gupta, V., Xuereb, P. A., & Buttigieg, S. C. Corporate Social Responsibility Application in the Healthcare Sector: A Bibliometric Analysis and Synthesis. International Journal of Information Systems and Social Change (IJISSC), 11(1), 11-23. Doi: 10.4018/IJISSC.2020010102 (2020) Many healthcare organizations recognize the importance of CSR in enhancing their reputation and contributing positively to society. Adopting sustainable practices aligns with CSR goals and demonstrates a commitment to ethical practices which results in a good image along the more conscious becoming public, so CSR is known to be vital to the corporate´s reputation.76Sherman, J. D., MacNeill, A. J., Biddinger, P. D., Ergun, O., Salas, R. N., & Eckelman, M. J. Sustainable and resilient health care in the face of a changing climate. Annual Review of Public Health, 44, 255-277. (2023) Sustainability practices also enhance healthcare organizations’ resilience to challenges such as natural disasters, disease outbreaks, and other emergencies as mentioned previously. Preparedness for such events contributes to the long-term stability of the healthcare system and is a preventative strategy.77Hu, H., Cohen, G., Sharma, B., Yin, H., & McConnell, R. Sustainability in Health Care. Annual Review of Environment and Resources, 47, 173-196. Another driver is research in sustainability, which has grown within the healthcare sector, leading to the identification of best practices and innovative solutions. Organizations are more likely to adopt sustainable practices when supported by evidence-based research.78WHO. Background paper for the regional technical consultation on: Monitoring the Health-Related Sustainable Development Goals (SDGs) SEARO, New Delhi, India. https://cdn.who.int/media/docs/default-source/searo/hsd/hwf/01-monitoring-the-health-related-sdgs-background-paper.pdf?sfvrsn=3417607a_4&download=true (2017) Furthermore, international efforts to improve healthcare access and quality often include sustainability considerations. As mentioned in Chapter 2: Background, Initiatives such as the Sustainable Development Goals (SDGs) emphasize the importance of sustainable healthcare systems in achieving broader global health objectives with SDG 3: “Good health and well-being: ensure healthy lives and promote well-being for all as all ages” in the center.79Patil, A., Shardeo, V., Dwivedi, A., Madaan, J., & Varma, N. Barriers to sustainability in humanitarian medical supply chains. Sustainable Production and Consumption, 27, 1794-1807. (2021)
These drivers mentioned above collectively encourage healthcare organizations to adopt sustainable practices that not only benefit the environment but also contribute to better patient care, cost efficiency, and long-term viability of the healthcare sector.
4.2 Barriers
On the other hand, there are significant barriers that the sustainable development in the healthcare sector must face which can hinder the adoption and implementation of sustainable practices. These barriers arise from a combination of economic, social, organizational, and regulatory factors.
Healthcare organizations are often faced with limited budgets, therefore limiting their ability to invest in sustainability initiatives. Some initiatives like implementing energy-efficient technologies or sustainable infrastructure can come with upfront costs. The perceived financial burden and also inconsistent engagement from various stakeholders can deter investment in these strategic changes and programs.80Leite, H., Bateman, N., & Radnor, Z. Beyond the ostensible: an exploration of barriers to lean implementation and sustainability in healthcare. Production Planning & Control, 31(1), 1-18. (2020) Besides, healthcare professionals and administrators may not fully understand the benefits of sustainable practices or may lack awareness about the environmental and social impacts of healthcare operations. Lack of education and awareness can hinder the motivation to adopt sustainable initiatives and therefore be a barrier. Additionally, healthcare organizations may prioritize immediate patient care needs over long-term sustainability efforts. The focus on addressing urgent health concerns might lead to neglecting sustainable practices.81Chate, A. B., Anikumar, E. N., & Sridharan, R. Analysis of barriers and enablers of sustainability implementation in healthcare centers. In Operations Management and Systems Engineering: Select Proceedings of CPIE 2019 (pp. 287-298). Springer Singapore. (2021)
Furthermore, implementing sustainability initiatives often requires changes in established workflows and practices and thus encounter resistance from staff, patients, and management, which can impede the adoption of new processes and technologies.82Leonidou, C. N., & Skarmeas, D. Gray shades of green: Causes and consequences of green skepticism. Journal of business ethics, 144, 401-415. (2017) Resistance to change and traditional practices can be deeply ingrained in the healthcare culture. Additionally, some healthcare professionals may doubt the effectiveness of sustainability efforts in improving patient care or reducing costs. A lack of clear evidence for the benefits of sustainable practices can contribute to skepticism.83Chiarini, A. and Vagnoni, E. (2016), “Environmental sustainability in European public healthcare: could it just be a matter of leadership?”, Leadership in Health Services, Vol. 29 No. 1, pp. 2-8. (2016) On top of that, healthcare regulations can be complex and vary across jurisdictions. Navigating the regulatory landscape while trying to adopt sustainable practices can be challenging and time-consuming. Despite the importance of managing its environmental impact, public healthcare only implements green standards to a limited extend, because adopting effective operational strategies is one of the biggest organizational challenges.84Evans, M. and Farrell, P. “A strategic framework managing challenges of integrating lean construction and integrated project delivery on construction megaprojects, towards global integrated delivery transformative initiatives in multinational organisations”, Journal of Engineering, Design and Technology, Vol. ahead-of-print. (2022) 85AlJaberi, O. A., Hussain, M., & Drake, P. R. A framework for measuring sustainability in healthcare systems. International journal of healthcare management. (2017) Measuring the environmental and social impacts of healthcare operations can also be difficult, due to the lack of standardized metrics and data collection systems. This hinders organizations from accurately assessing their progress towards sustainability goals.86Dion, H., & Evans, M. Strategic frameworks for sustainability and corporate governance in healthcare facilities; approaches to energy-efficient hospital management. Benchmarking: An International Journal. (2023) Older healthcare facilities may lack the infrastructure needed to implement energy-efficient technologies or waste management systems. Retrofitting existing infrastructure can be expensive and logistically complex.87Stevanovic, M., Allacker, K., & Vermeulen, S. Hospital building sustainability: The experience in using qualitative tools and steps towards the life cycle approach. Procedia environmental sciences, 38, 445-451. (2017) Healthcare organizations have numerous priorities, which can divert attention and resources away from sustainability initiatives.88University of Vermont Medical Center. Website: https://www.uvmhealth.org/healthsource/sustainability-remains-a-priority-uvm-medical-center#:~:text=UVM%20Medical%20Center%20currently%20recycles,the%20hospital%20during%20the%20pandemic. Complex organizational structures and decision-making processes in healthcare systems can slow down or complicate the adoption of sustainable practices. Decision-making involving multiple stakeholders may also lead to delays and pose as a barrier. Overcoming these barriers requires a concerted effort from healthcare leaders, professionals, policymakers, and stakeholders.
An example of a healthcare institution that overcame barriers to implement sustainability measures is the University of Vermont Medical Center (UVMMC), which faced challenges in reducing medical waste and single-use plastics. UVMMC made an effort and overcame that barrier by focusing on sustainable procurement practices, sourcing environmentally friendly products, working with suppliers to reduce packaging waste and implementing a program to replace plastic straws with paper straws as well as a comprehensive recycling program including proper disposal of medical waste.89University of Vermont Medical Center. Website: https://www.uvmhealth.org/healthsource/sustainability-remains-a-priority-uvm-medical-center#:~:text=UVM%20Medical%20Center%20currently%20recycles,the%20hospital%20during%20the%20pandemic.
The Cleveland Clinic in Ohio, USA, is a prime example of a hospital that conquered challenges in healthcare complexity, reliable power, and patient care priorities. The clinic’s commitment to sustainability is evident through its Office of Sustainability. Green building principles are embraced in new construction and renovations, like the energy-efficient Glickman Tower with natural light and recycled materials. They adopted LED lighting, efficient HVAC, and advanced management for reduced energy use and costs. Solar panels generate renewable energy, cutting reliance on non-renewables and shrinking their carbon footprint. Sustainable transport options include bike shares, EV charging and better public transit. Continuously assessing efforts, the clinic strives for greater environmental impact reduction. With a holistic approach, empowered leadership, and ongoing improvements, Cleveland Clinic stands as a model for sustainable healthcare.90Cleveland Clinic Ohio. Website: https://my.clevelandclinic.org/about/community/sustainability/sustainability-global-citizenship
In Germany, there is movement in the industry and some examples worth mentioning. The Evangelical Hospital Hubertus in Berlin produces its own energy and uses the efficiency of combined heat and power generation. The hospital is a pioneer when it comes to saving energy. By 2001, the facility had reduced its energy consumption by 37 percent and CO2 emissions by 2,600 tons. At the time, it was the first hospital in Germany to receive the “Energy-saving Hospital” seal of approval from the German Federation for the Environment and Nature Conservation (BUND).91Ärtzeblatt. Archiv. Nachhaltigkeit – Das grüne Krankenhaus. Website: https://www.aerzteblatt.de/archiv/147581/Nachhaltigkeit-Das-gruene-Krankenhaus (n.d.)
St. Marien Clinic in Amberg, Upper Palatinate, embraces comprehensive sustainability. With a history of over 160 years, the clinic addresses building age through strategic renovations. In 2011, they underwent a Siemens-developed “Green+ Check” assessment, surpassing BUND’s seal. This standardized method evaluates environment, quality, and efficiency aspects across energy, infrastructure, technology, and staff training. Comparisons with benchmarks yield a personalized sustainability index, highlighting strengths, weaknesses, and improvement opportunities. The VDE’s extension, the “Blue Hospital,” further refines this approach into a universal application rule. Some federal states such as Rhineland-Palatinate and Bavaria are now in the process of supporting their hospitals in switching to a sustainable energy and ecological standard. Rhineland-Palatinate wants to introduce a quality seal for sustainable hospitals. In Bavaria, the concept of the sustainable hospital is to be implemented across the board with the “Green Hospital Initiative”. The initiative includes a whole bundle of funding measures. Municipal hospitals receive financial support for advice on potential energy savings via the Bavarian CO2 reduction program.91Ärtzeblatt. Archiv. Nachhaltigkeit – Das grüne Krankenhaus. Website: https://www.aerzteblatt.de/archiv/147581/Nachhaltigkeit-Das-gruene-Krankenhaus (n.d.)
These examples show that the barriers of sustainability in healthcare can be overcome and even though there is still a lot to improve, and the goals are far from being achieved, a development into the right direction can be seen throughout the healthcare sector.
- 1Akbal, H., Doğan, N.Ö. Handbook of Research on Quality and Copmetitiveness in the Healthcare Services Sector. Chapter: Lean and Smart Supply Chain Management in Healthcare. Doi: 10.4018/978-1-6684-8103-5.ch002
(2023) - 2Dailey, J. W. (2023, July 21). Encyclopaedia Britannica. Pharmaceutical industry. https://www.britannica.com/technology/pharmaceutical-industry (2023)
- 3Aronson, J. K., Heneghan, C., & Ferner, R. E. Medical Devices: Definition, Classification, and Regulatory Implications. Drug safety, 43(2), 83–93. Doi: 10.1007/s40264-019-00878-3 (2020)
- 4Institute of Medicine (US) Committee on the Consequences of Uninsurance. Coverage Matters: Insurance and Health Care. Washington (DC): National Academies Press (US); 1, Why Health Insurance Matters. Available: https://www.ncbi.nlm.nih.gov/books/NBK223643/ (2001)
- 5Nutbeam, D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health promotion international, 15(3), 259-267. (2000)
- 6Marimuthu, M., & Paulose, H. Emergence of sustainability based approaches in healthcare: expanding research and practice. Procedia-Social and Behavioral Sciences, 224, 554-561. (2016)
- 7MOOSMANN et. al., The COP27 Climate Change Conference: status of climate negotiations and issues at stake. Available at: https://www.europarl.europa.eu/RegData/etudes/STUD/2022/733989/IPOL_STU(2022)733989_EN.pdf
- 8Brown, H. et. Al. The Energy Burden and Environmental Impact of Health Services. Am J Public Health. 2012 December; 102(12): e76–e82. doi: 10.2105/AJPH.2012.300776. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3519304/ (2012)
- 9Bratu, A., et. Al. The 2021 Western North American heat dome increased climate change anxiety among British Columbians: Results from a natural experiment. The Journal of Climate Change and Health, 6, 100116. (2022)
- 10Lugten, E., Hariharan, N. Strengthening Health Systems for Climate Adaption and Health Security: Key Considerations for Policy and Programming. Health Secur. September/October 2022; 20(5): 435–439. doi: 10.1089/hs.2022.0050. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9595646/ (2022)
- 11Hernández, A.-C. Reducing Healthcare´s Climate Footprint: Opportunities for European Hospitals & Health Systems. Available at: https://noharm-europe.org/sites/default/files/documents-files/4746/HCWHEurope_Climate_Report_Dec2016.pdf (2016)
- 12Jamieson, M., Wicks, A., & Boulding, T. Becoming environmentally sustainable in healthcare: an overview. Australian health review: a publication of the Australian Hospital Association, 39(4), 417–424. https://doi.org/10.1071/AH14086 (2015)
- 13McMichael, Anthony J. Globalization, Climate Change, and Human Health. The New England journal of medicine 368, 1335–1343 (2013)
- 14Keller et. al. From bandages to buildings: Identifying the environmental hotspots of hospitals. Journal of Cleaner Production 319, 2-12 (2021)
- 15Health Care Without Harm in collaboration with Arup. Health Care’s Climate Footprint (2019)
- 16Walia et. al. Quantitation of antibiotic resistance genes pollution in hospital waste water effluent and Urban Clinton River Water, Michigan, USA. Current Medicine Research and Practice 6, 149–151 (2016)
- 17Janik-Karpinska et. al. Healthcare Waste – A Serious Problem for Global Health. Healthcare (Basel, Switzerland) 11, 242 (2023)
- 18Pankaj C. et.al. Role of Industries in Water Scarcity and Its Adverse Effects on Environment and Human Health in Environmental Concerns and Sustainable Development (eds. Shukla, V; Kumar, N.) 235-256 (Springer, 2020)
- 19McGain et. al. An audit of intensive care unit recyclable waste. Anaesthesia 64, 1299–1302 (2009)
- 20Kanning, H. Managementregeln der Nachhaltigkeit in Betriebliches Nachhaltigkeitsmanagement (eds. Baumast; Pape) 33-34 (UTB; Verlag Eugen Ulmer 2022)
- 21Bodensee-Stiftung and Global Nature Fund. Leitfaden 2023 – Schutz der biologischen Vielfalt im Rahmen von Umweltmanagementsystemen (2023)
- 22Magis, K.; Shinn, C. Emerging Principles of Social Sustainability in Understanding the Social Dimension of Sustainability (eds. Dillard et. al.) 15-44 (Routledge, 2009)
- 23Mousa et. al. Advancing women in healthcare leadership: A systematic review and meta-synthesis of multi-sector evidence on organisational interventions. EClinicalMedicine 39, 101084 (2021)
- 24Stanford; Fatima. The Importance of Diversity and Inclusion in the Healthcare Workforce. Journal of the National Medical Association 112, 247–249 (2020)
- 25Deshpande, Satish P. A Study of Ethical Decision Making by Physicians and Nurses in Hospitals. Journal of Business Ethics 90, 387–397 (2009)
- 26Kcomt L. et. al. Healthcare avoidance due to anticipated discrimination among transgender people: A call to create trans-affirmative environments. SSM – population health 11, 100608 (2020)
- 27Geiger-Brown, J.; Lipscomb, J. The Health Care Work Environment and Adverse Health and Safety Consequences for Nurses. Annual review of nursing research 28, 191–231 (2010)
- 28Rathert, C.; May, D. R. Health care work environments, employee satisfaction, and patient safety. Health Care Management Review 32, 2-11 (2007)
- 29The International Labor Organization and the World Health Organization. The gender pay gap in the health and care sector (2022)
- 30KFF. Health Care Employment as a Percent of Total Employment https://www.kff.org/other/state-indicator/health-care-employment-as-total (2022)
- 31Bundesgesundheitsministerium. Personal in der Gesundheitswirtschaft https://www.bundesgesundheitsministerium.de/fileadmin/Dateien/2_Bilder/2_Grafiken/Infografiken/Gesundheit/Infografik_Gesundheitspersonal.pdf (2023)
- 32Heled et. al. The problem with relying on profit-driven models to produce pandemic drugs. Journal of law and the biosciences 7, 1–23 (2023)
- 33Preeti Vankar. Health expenditure as a percentage of gross domestic product (GDP) in selected countries in 2022. Statista https://www.statista.com/statistics/268826/health-expenditure-as-gdp-percentage-in-oecd-countries/ (2022)
- 34International Standards Organization. ISO 14001 Environmental Management Systems (2015)
- 35Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health 57, p.1768 (2021)
- 36Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.1 (2019)
- 37World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.3 (2009)
- 38Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.2 (2019)
- 39World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.10 (2009)
- 40Health Care Without Harm and Practice Greenhealth: Adressing Climate Change in the Health Care Setting, p.6-7. (n.d.)
- 41Altin, A. & Altin, S.: Sustainable Water and Wastewater Management in Hospitals, in: The Turkish Journal of Occupational / Environmental Medicine and Safety 2 (1), p.2 (2007)
- 42Zhu, Q., Johnson, S. & Sarkis, J.: Lean six sigma and environmental sustainability: a hospital perspective, in: Supply Chain Forum: An International Journal, p.4 (2018)
- 43Bross, L. et. al.: Public health without water? Emergency water supply and minimum supply standards of hospitals in high-income countries using the example of Germany and Austria, in: Water Policy 23 (2), p.1 (2021)
- 44Verlicchi, P. et. al.: Hospital effluents as a source of emerging pollutants: An overview of micropollutants and sustainable treatment options, in: Journal of Hydrology 389, p.1 (2010)
- 45Altin, A. & Altin, S.: Sustainable Water and Wastewater Management in Hospitals, in: The Turkish Journal of Occupational / Environmental Medicine and Safety 2 (1), p.6 (2007)
- 46World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.21 (2009)
- 48Health Care Without Harm and Practice Greenhealth: Adressing Climate Change in the Health Care Setting, p.10. (n.d.)
- 49World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.19 (2009).
- 50Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health 57, p.1771 (2021)
- 51EPA Carbon Pollution from Transportation https://www.epa.gov/transportation-air-pollution-and-climate-change/carbon-pollution-transportation
- 52Health Care Without Harm and Practice Greenhealth: Adressing Climate Change in the Health Care Setting, p.5. (n.d.)
- 53Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health 57, p.1772 (2021)
- 54World Health Organization: Health in the green Economy, Health Care Facilities, p.2 (2011)
- 55Hu et. al. : Sustainability in Health Care, in: Annual Review of Environment and Resources 47, p.183 (2022)
- 56Mehra, R. & Sharma, M. K.: Measures of Sustainability in Healthcare, in: Sustainability Analytics and Modeling 1, p.2 (2021)
- 57World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.12 (2009)
- 58Langstaff, K. & Brzozowski, V.: Managing environmental sustainability in a healthcare setting, in: Healthcare Management Forum 30(2), p. 86 (2017)
- 59Health Care Without Harm and Practice Greenhealth: Adressing Climate Change in the Health Care Setting, p.8. (n.d.)
- 60Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health 57, p.1767 (2021)
- 61Mehra, R. & Sharma, M. K.: Measures of Sustainability in Healthcare, in: Sustainability Analytics and Modeling 1, p.1 (2021)
- 62Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.1-2 (2019)
- 63Zhu, Q., Johnson, S. & Sarkis, J.: Lean six sigma and environmental sustainability: a hospital perspective, in: Supply Chain Forum: An International Journal, p.3 (2018)
- 64Langstaff, K. & Brzozowski, V.: Managing environmental sustainability in a healthcare setting, in: Healthcare Management Forum 30(2), p. 84 (2017)
- 65Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.4 (2019)
- 66Hu et. al. : Sustainability in Health Care, in: Annual Review of Environment and Resources 47, p.180 (2022)
- 67Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.3 (2019)
- 68Health Care Without Harm and Practice Greenhealth: Adressing Climate Change in the Health Care Setting, p.9. (n.d.)
- 69European Commission. Website:https://climate.ec.europa.eu/climate-change/consequences-climate-change_en (2023)
- 70Government of the Netherlands. Sustainable Healthcare. Website: https://www.government.nl/topics/sustainable-healthcare/more-sustainability-in-the-care-sector#:~:text=The%203rd%20Green%20Deal%20on,on%20climate%20and%20the%20environment. (2023)
- 71WHO guidance for climate-resilient and environmentally sustainable health care facilities. Geneva: World Health Organization; Licence: CC BY-NC-SA 3.0 IGO. (2020)
- 72Sherman, J. et.al. The Green Print: Advancement of Environmental Sustainability in Healthcare, Resources, Conservation and Recycling, Volume 161, 104882, ISSN 0921-3449, Doi: 10.1016/j.resconrec.2020.104882. (2020)
- 73Arab ul Mateen, Qasim Ali Nisar, Nadia Nasir, Fostering pro-environmental behaviors in the healthcare organizations: An empirical analysis of psychological and strategic factors, Asia Pacific Management Review, Volume 28, Issue 1, Pages 13-23, ISSN 1029-3132, Doi: 10.1016/j.apmrv.2022.01.004., (2023)
- 74Kruk, M. E., et. al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. The Lancet. Global health, 6(11), e1196–e1252. Doi: 10.1016/S2214-109X(18)30386-3(2018)
- 75Tomaselli, G., Garg, L., Gupta, V., Xuereb, P. A., & Buttigieg, S. C. Corporate Social Responsibility Application in the Healthcare Sector: A Bibliometric Analysis and Synthesis. International Journal of Information Systems and Social Change (IJISSC), 11(1), 11-23. Doi: 10.4018/IJISSC.2020010102 (2020)
- 76Sherman, J. D., MacNeill, A. J., Biddinger, P. D., Ergun, O., Salas, R. N., & Eckelman, M. J. Sustainable and resilient health care in the face of a changing climate. Annual Review of Public Health, 44, 255-277. (2023)
- 77Hu, H., Cohen, G., Sharma, B., Yin, H., & McConnell, R. Sustainability in Health Care. Annual Review of Environment and Resources, 47, 173-196.
- 78WHO. Background paper for the regional technical consultation on: Monitoring the Health-Related Sustainable Development Goals (SDGs) SEARO, New Delhi, India. https://cdn.who.int/media/docs/default-source/searo/hsd/hwf/01-monitoring-the-health-related-sdgs-background-paper.pdf?sfvrsn=3417607a_4&download=true (2017)
- 79Patil, A., Shardeo, V., Dwivedi, A., Madaan, J., & Varma, N. Barriers to sustainability in humanitarian medical supply chains. Sustainable Production and Consumption, 27, 1794-1807. (2021)
- 80Leite, H., Bateman, N., & Radnor, Z. Beyond the ostensible: an exploration of barriers to lean implementation and sustainability in healthcare. Production Planning & Control, 31(1), 1-18. (2020)
- 81Chate, A. B., Anikumar, E. N., & Sridharan, R. Analysis of barriers and enablers of sustainability implementation in healthcare centers. In Operations Management and Systems Engineering: Select Proceedings of CPIE 2019 (pp. 287-298). Springer Singapore. (2021)
- 82Leonidou, C. N., & Skarmeas, D. Gray shades of green: Causes and consequences of green skepticism. Journal of business ethics, 144, 401-415. (2017)
- 83Chiarini, A. and Vagnoni, E. (2016), “Environmental sustainability in European public healthcare: could it just be a matter of leadership?”, Leadership in Health Services, Vol. 29 No. 1, pp. 2-8. (2016)
- 84Evans, M. and Farrell, P. “A strategic framework managing challenges of integrating lean construction and integrated project delivery on construction megaprojects, towards global integrated delivery transformative initiatives in multinational organisations”, Journal of Engineering, Design and Technology, Vol. ahead-of-print. (2022)
- 85AlJaberi, O. A., Hussain, M., & Drake, P. R. A framework for measuring sustainability in healthcare systems. International journal of healthcare management. (2017)
- 86Dion, H., & Evans, M. Strategic frameworks for sustainability and corporate governance in healthcare facilities; approaches to energy-efficient hospital management. Benchmarking: An International Journal. (2023)
- 87Stevanovic, M., Allacker, K., & Vermeulen, S. Hospital building sustainability: The experience in using qualitative tools and steps towards the life cycle approach. Procedia environmental sciences, 38, 445-451. (2017)
- 88University of Vermont Medical Center. Website: https://www.uvmhealth.org/healthsource/sustainability-remains-a-priority-uvm-medical-center#:~:text=UVM%20Medical%20Center%20currently%20recycles,the%20hospital%20during%20the%20pandemic.
- 89University of Vermont Medical Center. Website: https://www.uvmhealth.org/healthsource/sustainability-remains-a-priority-uvm-medical-center#:~:text=UVM%20Medical%20Center%20currently%20recycles,the%20hospital%20during%20the%20pandemic.
- 90Cleveland Clinic Ohio. Website: https://my.clevelandclinic.org/about/community/sustainability/sustainability-global-citizenship
- 91Ärtzeblatt. Archiv. Nachhaltigkeit – Das grüne Krankenhaus. Website: https://www.aerzteblatt.de/archiv/147581/Nachhaltigkeit-Das-gruene-Krankenhaus (n.d.)
[i] Akbal, H., Doğan, N.Ö. Handbook of Research on Quality and Copmetitiveness in the Healthcare Services Sector. Chapter: Lean and Smart Supply Chain Management in Healthcare. Doi: 10.4018/978-1-6684-8103-5.ch002
(2023)
[ii] Dailey, J. W. (2023, July 21). Encyclopaedia Britannica. Pharmaceutical industry. https://www.britannica.com/technology/pharmaceutical-industry (2023)
[iii] Aronson, J. K., Heneghan, C., & Ferner, R. E. Medical Devices: Definition, Classification, and Regulatory Implications. Drug safety, 43(2), 83–93. Doi: 10.1007/s40264-019-00878-3 (2020)
[iv] Institute of Medicine (US) Committee on the Consequences of Uninsurance. Coverage Matters: Insurance and Health Care. Washington (DC): National Academies Press (US); 1, Why Health Insurance Matters. Available: https://www.ncbi.nlm.nih.gov/books/NBK223643/ (2001)
[v] Nutbeam, D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health promotion international, 15(3), 259-267. (2000)
[vi] Marimuthu, M., & Paulose, H. Emergence of sustainability based approaches in healthcare: expanding research and practice. Procedia-Social and Behavioral Sciences, 224, 554-561. (2016)
[vii] MOOSMANN et. al., The COP27 Climate Change Conference: status of climate negotiations and issues at stake. Available at: https://www.europarl.europa.eu/RegData/etudes/STUD/2022/733989/IPOL_STU(2022)733989_EN.pdf
[viii] Brown, H. et. Al. The Energy Burden and Environmental Impact of Health Services. Am J Public Health. 2012 December; 102(12): e76–e82. doi: 10.2105/AJPH.2012.300776. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3519304/ (2012)
[ix] Bratu, A., et. Al. The 2021 Western North American heat dome increased climate change anxiety among British Columbians: Results from a natural experiment. The Journal of Climate Change and Health, 6, 100116. (2022)
[x] Lugten, E., Hariharan, N. Strengthening Health Systems for Climate Adaption and Health Security: Key Considerations for Policy and Programming. Health Secur. September/October 2022; 20(5): 435–439. doi: 10.1089/hs.2022.0050. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9595646/ (2022)
[xi] Hernández, A.-C. Reducing Healthcare´s Climate Footprint: Opportunities for European Hospitals & Health Systems. Available at: https://noharm-europe.org/sites/default/files/documents-files/4746/HCWHEurope_Climate_Report_Dec2016.pdf (2016)
[xii] Jamieson, M., Wicks, A., & Boulding, T. Becoming environmentally sustainable in healthcare: an overview. Australian health review: a publication of the Australian Hospital Association, 39(4), 417–424. https://doi.org/10.1071/AH14086 (2015)
[xiii] McMichael, Anthony J. Globalization, Climate Change, and Human Health. The New England journal of medicine 368, 1335–1343 (2013)
[xiv] Keller et. al. From bandages to buildings: Identifying the environmental hotspots of hospitals. Journal of Cleaner Production 319, 2-12 (2021)
[xv] Keller et. al. From bandages to buildings: Identifying the environmental hotspots of hospitals. Journal of Cleaner Production 319, 2-12 (2021)
[xvi] Health Care Without Harm in collaboration with Arup. Health Care’s Climate Footprint (2019)
[xvii] Walia et. al. Quantitation of antibiotic resistance genes pollution in hospital waste water effluent and Urban Clinton River Water, Michigan, USA. Current Medicine Research and Practice 6, 149–151 (2016)
[xviii] Janik-Karpinska et. al. Healthcare Waste – A Serious Problem for Global Health. Healthcare (Basel, Switzerland) 11, 242 (2023)
[xix] Health Care Without Harm in collaboration with Arup. Health Care’s Climate Footprint (2019)
[xx] Pankaj C. et.al. Role of Industries in Water Scarcity and Its Adverse Effects on Environment and Human Health in Environmental Concerns and Sustainable Development (eds. Shukla, V; Kumar, N.) 235-256 (Springer, 2020)
[xxi] McGain et. al. An audit of intensive care unit recyclable waste. Anaesthesia 64, 1299–1302 (2009)
[xxii] Kanning, H. Managementregeln der Nachhaltigkeit in Betriebliches Nachhaltigkeitsmanagement (eds. Baumast; Pape) 33-34 (UTB; Verlag Eugen Ulmer 2022)
[xxiii] Bodensee-Stiftung and Global Nature Fund. Leitfaden 2023 – Schutz der biologischen Vielfalt im Rahmen von Umweltmanagementsystemen (2023)
[xxiv] Magis, K.; Shinn, C. Emerging Principles of Social Sustainability in Understanding the Social Dimension of Sustainability (eds. Dillard et. al.) 15-44 (Routledge, 2009)
[xxv] Department of Economic and Social Affairs, Sustainable Development. The 17 SDGs. United Nations. https://sdgs.un.org/goals (2023)
[xxvi] Stanford; Fatima. The Importance of Diversity and Inclusion in the Healthcare Workforce. Journal of the National Medical Association 112, 247–249 (2020)
[xxvii] Deshpande, Satish P. A Study of Ethical Decision Making by Physicians and Nurses in Hospitals. Journal of Business Ethics 90, 387–397 (2009)
[xxviii] Mousa et. al. Advancing women in healthcare leadership: A systematic review and meta-synthesis of multi-sector evidence on organisational interventions. EClinicalMedicine 39, 101084 (2021)
[xxix] Mousa et. al. Advancing women in healthcare leadership: A systematic review and meta-synthesis of multi-sector evidence on organisational interventions. EClinicalMedicine 39, 101084 (2021)
[xxx] Kcomt L. et. al. Healthcare avoidance due to anticipated discrimination among transgender people: A call to create trans-affirmative environments. SSM – population health 11, 100608 (2020)
[xxxi] Geiger-Brown, J.; Lipscomb, J. The Health Care Work Environment and Adverse Health and Safety Consequences for Nurses. Annual review of nursing research 28, 191–231 (2010)
[xxxii] Rathert, C.; May, D. R. Health care work environments, employee satisfaction, and patient safety. Health Care Management Review 32, 2-11 (2007)
[xxxiii] The International Labor Organization and the World Health Organization. The gender pay gap in the health and care sector (2022)
[xxxiv] KFF. Health Care Employment as a Percent of Total Employment https://www.kff.org/other/state-indicator/health-care-employment-as-total (2022)
[xxxv] Bundesgesundheitsministerium. Personal in der Gesundheitswirtschaft https://www.bundesgesundheitsministerium.de/fileadmin/Dateien/2_Bilder/2_Grafiken/Infografiken/Gesundheit/Infografik_Gesundheitspersonal.pdf (2023)
[xxxvi] Heled et. al. The problem with relying on profit-driven models to produce pandemic drugs. Journal of law and the biosciences 7, 1–23 (2023)
[xxxvii] Preeti Vankar. Health expenditure as a percentage of gross domestic product (GDP) in selected countries in 2022. Statista https://www.statista.com/statistics/268826/health-expenditure-as-gdp-percentage-in-oecd-countries/ (2022)
[xxxviii] International Standards Organization. ISO 14001 Environmental Management Systems (2015)
[xxxix] Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health 57, p.1768 (2021)
[xl] Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health no.57, p.1767 (2021)
[xli] Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health 57, p.1768 (2021)
[xlii] Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.1 (2019)
[xliii] Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health 57, p.1769-1770 (2021)
[xliv] Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health 57, p.1770 (2021)
[xlv] World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.3 (2009)
[xlvi] Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.2 (2019)
[xlvii] World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.10 (2009)
[xlviii] Health Care Without Harm and Practice Greenhealth: Adressing Climate Change in the Health Care Setting, p.6-7. (n.d.)
[xlix] World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.10 (2009)
[l] Altin, A. & Altin, S.: Sustainable Water and Wastewater Management in Hospitals, in: The Turkish Journal of Occupational / Environmental Medicine and Safety 2 (1), p.2 (2007)
[li] Zhu, Q., Johnson, S. & Sarkis, J.: Lean six sigma and environmental sustainability: a hospital perspective, in: Supply Chain Forum: An International Journal, p.4 (2018)
[lii] Bross, L. et. al.: Public health without water? Emergency water supply and minimum supply standards of hospitals in high-income countries using the example of Germany and Austria, in: Water Policy 23 (2), p.1 (2021)
[liii] Verlicchi, P. et. al.: Hospital effluents as a source of emerging pollutants: An overview of micropollutants and sustainable treatment options, in: Journal of Hydrology 389, p.1 (2010)
[liv] Altin, A. & Altin, S.: Sustainable Water and Wastewater Management in Hospitals, in: The Turkish Journal of Occupational / Environmental Medicine and Safety 2 (1), p.6 (2007)
[lv] World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.21 (2009)
[lvi] Health Care Without Harm and Practice Greenhealth: Adressing Climate Change in the Health Care Setting, p.10. (n.d.)
[lvii] Health Care Without Harm and Practice Greenhealth: Adressing Climate Change in the Health Care Setting, p.10. (n.d.)
[lviii] World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.19 (2009).
[lix] Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health 57, p.1771 (2021)
[lx] Health Care Without Harm and Practice Greenhealth: Adressing Climate Change in the Health Care Setting, p.10. (n.d.)
[lxi] EPA Carbon Pollution from Transportation https://www.epa.gov/transportation-air-pollution-and-climate-change/carbon-pollution-transportation
[lxii] Health Care Without Harm and Practice Greenhealth: Adressing Climate Change in the Health Care Setting, p.5. (n.d.)
[lxiii] Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health 57, p.1771 (2021)
[lxiv] Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health 57, p.1772 (2021)
[lxv] World Health Organization: Health in the green Economy, Health Care Facilities, p.2 (2011)
[lxvi] Hu et. al. : Sustainability in Health Care, in: Annual Review of Environment and Resources 47, p.183 (2022)
[lxvii] Mehra, R. & Sharma, M. K.: Measures of Sustainability in Healthcare, in: Sustainability Analytics and Modeling 1, p.2 (2021)
[lxviii] Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.2 (2019)
[lxix] World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.12 (2009)
[lxx] World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.12 (2009)
[lxxi] World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.12 (2009)
[lxxii] Langstaff, K. & Brzozowski, V.: Managing environmental sustainability in a healthcare setting, in: Healthcare Management Forum 30(2), p. 86 (2017)
[lxxiii] Health Care Without Harm and Practice Greenhealth: Adressing Climate Change in the Health Care Setting, p.8. (n.d.)
[lxxiv] Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health 57, p.1767 (2021)
[lxxv] Mehra, R. & Sharma, M. K.: Measures of Sustainability in Healthcare, in: Sustainability Analytics and Modeling 1, p.1 (2021)
[lxxvi] World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.10 (2009)
[lxxvii] Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.1-2 (2019)
[lxxviii] Zhu, Q., Johnson, S. & Sarkis, J.: Lean six sigma and environmental sustainability: a hospital perspective, in: Supply Chain Forum: An International Journal, p.3 (2018)
[lxxix] Hu et. al. : Sustainability in Health Care, in: Annual Review of Environment and Resources 47, p.183 (2022)
[lxxx] World Health Organization: Health in the green Economy, Health Care Facilities, p.2 (2011)
[lxxxi] Langstaff, K. & Brzozowski, V.: Managing environmental sustainability in a healthcare setting, in: Healthcare Management Forum 30(2), p. 84 (2017)
[lxxxii] Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.1 (2019)
[lxxxiii] Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.4 (2019)
[lxxxiv] Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.1 (2019)
[lxxxv] Hu et. al. : Sustainability in Health Care, in: Annual Review of Environment and Resources 47, p.180 (2022)
[lxxxvi] Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.2 (2019)
[lxxxvii] Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.2 (2019)
[lxxxviii] Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.3 (2019)
[lxxxix] Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.3 (2019)
[xc]Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.4 (2019)
[xci] Health Care Without Harm and Practice Greenhealth: Adressing Climate Change in the Health Care Setting, p.9. (n.d.)
[xcii] Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.3 (2019)
[xciii] European Commission. Website:https://climate.ec.europa.eu/climate-change/consequences-climate-change_en (2023)
[xciv] Government of the Netherlands. Sustainable Healthcare. Website: https://www.government.nl/topics/sustainable-healthcare/more-sustainability-in-the-care-sector#:~:text=The%203rd%20Green%20Deal%20on,on%20climate%20and%20the%20environment. (2023)
[xcv] WHO guidance for climate-resilient and environmentally sustainable health care facilities. Geneva: World Health Organization; Licence: CC BY-NC-SA 3.0 IGO. (2020)
[xcvi] Sherman, J. et.al. The Green Print: Advancement of Environmental Sustainability in Healthcare, Resources, Conservation and Recycling, Volume 161, 104882, ISSN 0921-3449, Doi: 10.1016/j.resconrec.2020.104882. (2020)
[xcvii] Arab ul Mateen, Qasim Ali Nisar, Nadia Nasir, Fostering pro-environmental behaviors in the healthcare organizations: An empirical analysis of psychological and strategic factors, Asia Pacific Management Review, Volume 28, Issue 1, Pages 13-23, ISSN 1029-3132, Doi: 10.1016/j.apmrv.2022.01.004., (2023)
[xcviii] Kruk, M. E., et. al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. The Lancet. Global health, 6(11), e1196–e1252. Doi: 10.1016/S2214-109X(18)30386-3 (2018)
[xcix] Tomaselli, G., Garg, L., Gupta, V., Xuereb, P. A., & Buttigieg, S. C. Corporate Social Responsibility Application in the Healthcare Sector: A Bibliometric Analysis and Synthesis. International Journal of Information Systems and Social Change (IJISSC), 11(1), 11-23. Doi: 10.4018/IJISSC.2020010102 (2020)
[c] Sherman, J. D., MacNeill, A. J., Biddinger, P. D., Ergun, O., Salas, R. N., & Eckelman, M. J. Sustainable and resilient health care in the face of a changing climate. Annual Review of Public Health, 44, 255-277. (2023)
[ci] Hu, H., Cohen, G., Sharma, B., Yin, H., & McConnell, R. Sustainability in Health Care. Annual Review of Environment and Resources, 47, 173-196.
[cii] WHO. Background paper for the regional technical consultation on: Monitoring the Health-Related Sustainable Development Goals (SDGs) SEARO, New Delhi, India. https://cdn.who.int/media/docs/default-source/searo/hsd/hwf/01-monitoring-the-health-related-sdgs-background-paper.pdf?sfvrsn=3417607a_4&download=true (2017)
[ciii] Patil, A., Shardeo, V., Dwivedi, A., Madaan, J., & Varma, N. Barriers to sustainability in humanitarian medical supply chains. Sustainable Production and Consumption, 27, 1794-1807. (2021)
[civ] Leite, H., Bateman, N., & Radnor, Z. Beyond the ostensible: an exploration of barriers to lean implementation and sustainability in healthcare. Production Planning & Control, 31(1), 1-18. (2020)
[cv] Chate, A. B., Anikumar, E. N., & Sridharan, R. Analysis of barriers and enablers of sustainability implementation in healthcare centers. In Operations Management and Systems Engineering: Select Proceedings of CPIE 2019 (pp. 287-298). Springer Singapore. (2021)
[cvi] Leonidou, C. N., & Skarmeas, D. Gray shades of green: Causes and consequences of green skepticism. Journal of business ethics, 144, 401-415. (2017)
[cvii] Chiarini, A. and Vagnoni, E. (2016), “Environmental sustainability in European public healthcare: could it just be a matter of leadership?”, Leadership in Health Services, Vol. 29 No. 1, pp. 2-8. (2016)
[cviii] Evans, M. and Farrell, P. “A strategic framework managing challenges of integrating lean construction and integrated project delivery on construction megaprojects, towards global integrated delivery transformative initiatives in multinational organisations”, Journal of Engineering, Design and Technology, Vol. ahead-of-print. (2022)
[cix] AlJaberi, O. A., Hussain, M., & Drake, P. R. A framework for measuring sustainability in healthcare systems. International journal of healthcare management. (2017)
[cx] Dion, H., & Evans, M. Strategic frameworks for sustainability and corporate governance in healthcare facilities; approaches to energy-efficient hospital management. Benchmarking: An International Journal. (2023)
[cxi] Stevanovic, M., Allacker, K., & Vermeulen, S. Hospital building sustainability: The experience in using qualitative tools and steps towards the life cycle approach. Procedia environmental sciences, 38, 445-451. (2017)
[cxii] University of Vermont Medical Center. Website: https://www.uvmhealth.org/healthsource/sustainability-remains-a-priority-uvm-medical-center#:~:text=UVM%20Medical%20Center%20currently%20recycles,the%20hospital%20during%20the%20pandemic.
[cxiii] Cleveland Clinic Ohio. Website: https://my.clevelandclinic.org/about/community/sustainability/sustainability-global-citizenship
[cxiv] Ärtzeblatt. Archiv. Nachhaltigkeit – Das grüne Krankenhaus. Website: https://www.aerzteblatt.de/archiv/147581/Nachhaltigkeit-Das-gruene-Krankenhaus (n.d.)
[cxv] Ärtzeblatt. Archiv. Nachhaltigkeit – Das grüne Krankenhaus. Website: https://www.aerzteblatt.de/archiv/147581/Nachhaltigkeit-Das-gruene-Krankenhaus (n.d.)
- 1Akbal, H., Doğan, N.Ö. Handbook of Research on Quality and Copmetitiveness in the Healthcare Services Sector. Chapter: Lean and Smart Supply Chain Management in Healthcare. Doi: 10.4018/978-1-6684-8103-5.ch002
(2023) - 2Dailey, J. W. (2023, July 21). Encyclopaedia Britannica. Pharmaceutical industry. https://www.britannica.com/technology/pharmaceutical-industry (2023)
- 3Aronson, J. K., Heneghan, C., & Ferner, R. E. Medical Devices: Definition, Classification, and Regulatory Implications. Drug safety, 43(2), 83–93. Doi: 10.1007/s40264-019-00878-3 (2020)
- 4Institute of Medicine (US) Committee on the Consequences of Uninsurance. Coverage Matters: Insurance and Health Care. Washington (DC): National Academies Press (US); 1, Why Health Insurance Matters. Available: https://www.ncbi.nlm.nih.gov/books/NBK223643/ (2001)
- 5Nutbeam, D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health promotion international, 15(3), 259-267. (2000)
- 6Marimuthu, M., & Paulose, H. Emergence of sustainability based approaches in healthcare: expanding research and practice. Procedia-Social and Behavioral Sciences, 224, 554-561. (2016)
- 7MOOSMANN et. al., The COP27 Climate Change Conference: status of climate negotiations and issues at stake. Available at: https://www.europarl.europa.eu/RegData/etudes/STUD/2022/733989/IPOL_STU(2022)733989_EN.pdf
- 8Brown, H. et. Al. The Energy Burden and Environmental Impact of Health Services. Am J Public Health. 2012 December; 102(12): e76–e82. doi: 10.2105/AJPH.2012.300776. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3519304/ (2012)
- 9Bratu, A., et. Al. The 2021 Western North American heat dome increased climate change anxiety among British Columbians: Results from a natural experiment. The Journal of Climate Change and Health, 6, 100116. (2022)
- 10Lugten, E., Hariharan, N. Strengthening Health Systems for Climate Adaption and Health Security: Key Considerations for Policy and Programming. Health Secur. September/October 2022; 20(5): 435–439. doi: 10.1089/hs.2022.0050. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9595646/ (2022)
- 11Hernández, A.-C. Reducing Healthcare´s Climate Footprint: Opportunities for European Hospitals & Health Systems. Available at: https://noharm-europe.org/sites/default/files/documents-files/4746/HCWHEurope_Climate_Report_Dec2016.pdf (2016)
- 12Jamieson, M., Wicks, A., & Boulding, T. Becoming environmentally sustainable in healthcare: an overview. Australian health review: a publication of the Australian Hospital Association, 39(4), 417–424. https://doi.org/10.1071/AH14086 (2015)
- 13McMichael, Anthony J. Globalization, Climate Change, and Human Health. The New England journal of medicine 368, 1335–1343 (2013)
- 14Keller et. al. From bandages to buildings: Identifying the environmental hotspots of hospitals. Journal of Cleaner Production 319, 2-12 (2021)
- 15Health Care Without Harm in collaboration with Arup. Health Care’s Climate Footprint (2019)
- 16Walia et. al. Quantitation of antibiotic resistance genes pollution in hospital waste water effluent and Urban Clinton River Water, Michigan, USA. Current Medicine Research and Practice 6, 149–151 (2016)
- 17Janik-Karpinska et. al. Healthcare Waste – A Serious Problem for Global Health. Healthcare (Basel, Switzerland) 11, 242 (2023)
- 18Pankaj C. et.al. Role of Industries in Water Scarcity and Its Adverse Effects on Environment and Human Health in Environmental Concerns and Sustainable Development (eds. Shukla, V; Kumar, N.) 235-256 (Springer, 2020)
- 19McGain et. al. An audit of intensive care unit recyclable waste. Anaesthesia 64, 1299–1302 (2009)
- 20Kanning, H. Managementregeln der Nachhaltigkeit in Betriebliches Nachhaltigkeitsmanagement (eds. Baumast; Pape) 33-34 (UTB; Verlag Eugen Ulmer 2022)
- 21Bodensee-Stiftung and Global Nature Fund. Leitfaden 2023 – Schutz der biologischen Vielfalt im Rahmen von Umweltmanagementsystemen (2023)
- 22Magis, K.; Shinn, C. Emerging Principles of Social Sustainability in Understanding the Social Dimension of Sustainability (eds. Dillard et. al.) 15-44 (Routledge, 2009)
- 23Mousa et. al. Advancing women in healthcare leadership: A systematic review and meta-synthesis of multi-sector evidence on organisational interventions. EClinicalMedicine 39, 101084 (2021)
- 24Stanford; Fatima. The Importance of Diversity and Inclusion in the Healthcare Workforce. Journal of the National Medical Association 112, 247–249 (2020)
- 25Deshpande, Satish P. A Study of Ethical Decision Making by Physicians and Nurses in Hospitals. Journal of Business Ethics 90, 387–397 (2009)
- 26Kcomt L. et. al. Healthcare avoidance due to anticipated discrimination among transgender people: A call to create trans-affirmative environments. SSM – population health 11, 100608 (2020)
- 27Geiger-Brown, J.; Lipscomb, J. The Health Care Work Environment and Adverse Health and Safety Consequences for Nurses. Annual review of nursing research 28, 191–231 (2010)
- 28Rathert, C.; May, D. R. Health care work environments, employee satisfaction, and patient safety. Health Care Management Review 32, 2-11 (2007)
- 29The International Labor Organization and the World Health Organization. The gender pay gap in the health and care sector (2022)
- 30KFF. Health Care Employment as a Percent of Total Employment https://www.kff.org/other/state-indicator/health-care-employment-as-total (2022)
- 31Bundesgesundheitsministerium. Personal in der Gesundheitswirtschaft https://www.bundesgesundheitsministerium.de/fileadmin/Dateien/2_Bilder/2_Grafiken/Infografiken/Gesundheit/Infografik_Gesundheitspersonal.pdf (2023)
- 32Heled et. al. The problem with relying on profit-driven models to produce pandemic drugs. Journal of law and the biosciences 7, 1–23 (2023)
- 33Preeti Vankar. Health expenditure as a percentage of gross domestic product (GDP) in selected countries in 2022. Statista https://www.statista.com/statistics/268826/health-expenditure-as-gdp-percentage-in-oecd-countries/ (2022)
- 34International Standards Organization. ISO 14001 Environmental Management Systems (2015)
- 35Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health 57, p.1768 (2021)
- 36Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.1 (2019)
- 37World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.3 (2009)
- 38Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.2 (2019)
- 39World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.10 (2009)
- 40Health Care Without Harm and Practice Greenhealth: Adressing Climate Change in the Health Care Setting, p.6-7. (n.d.)
- 41Altin, A. & Altin, S.: Sustainable Water and Wastewater Management in Hospitals, in: The Turkish Journal of Occupational / Environmental Medicine and Safety 2 (1), p.2 (2007)
- 42Zhu, Q., Johnson, S. & Sarkis, J.: Lean six sigma and environmental sustainability: a hospital perspective, in: Supply Chain Forum: An International Journal, p.4 (2018)
- 43Bross, L. et. al.: Public health without water? Emergency water supply and minimum supply standards of hospitals in high-income countries using the example of Germany and Austria, in: Water Policy 23 (2), p.1 (2021)
- 44Verlicchi, P. et. al.: Hospital effluents as a source of emerging pollutants: An overview of micropollutants and sustainable treatment options, in: Journal of Hydrology 389, p.1 (2010)
- 45Altin, A. & Altin, S.: Sustainable Water and Wastewater Management in Hospitals, in: The Turkish Journal of Occupational / Environmental Medicine and Safety 2 (1), p.6 (2007)
- 46World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.21 (2009)
- 48Health Care Without Harm and Practice Greenhealth: Adressing Climate Change in the Health Care Setting, p.10. (n.d.)
- 49World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.19 (2009).
- 50Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health 57, p.1771 (2021)
- 51EPA Carbon Pollution from Transportation https://www.epa.gov/transportation-air-pollution-and-climate-change/carbon-pollution-transportation
- 52Health Care Without Harm and Practice Greenhealth: Adressing Climate Change in the Health Care Setting, p.5. (n.d.)
- 53Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health 57, p.1772 (2021)
- 54World Health Organization: Health in the green Economy, Health Care Facilities, p.2 (2011)
- 55Hu et. al. : Sustainability in Health Care, in: Annual Review of Environment and Resources 47, p.183 (2022)
- 56Mehra, R. & Sharma, M. K.: Measures of Sustainability in Healthcare, in: Sustainability Analytics and Modeling 1, p.2 (2021)
- 57World Health Organization and Health Care Without Harm: Healthy Hospitals, Healthy Planet, Healthy People, p.12 (2009)
- 58Langstaff, K. & Brzozowski, V.: Managing environmental sustainability in a healthcare setting, in: Healthcare Management Forum 30(2), p. 86 (2017)
- 59Health Care Without Harm and Practice Greenhealth: Adressing Climate Change in the Health Care Setting, p.8. (n.d.)
- 60Kiang, K.M & Behne, C.: Delivering environmental sustainability in healthcare for future generations: Time to clean up or own cubby house, in: Journal of Paediatrics and Child Health 57, p.1767 (2021)
- 61Mehra, R. & Sharma, M. K.: Measures of Sustainability in Healthcare, in: Sustainability Analytics and Modeling 1, p.1 (2021)
- 62Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.1-2 (2019)
- 63Zhu, Q., Johnson, S. & Sarkis, J.: Lean six sigma and environmental sustainability: a hospital perspective, in: Supply Chain Forum: An International Journal, p.3 (2018)
- 64Langstaff, K. & Brzozowski, V.: Managing environmental sustainability in a healthcare setting, in: Healthcare Management Forum 30(2), p. 84 (2017)
- 65Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.4 (2019)
- 66Hu et. al. : Sustainability in Health Care, in: Annual Review of Environment and Resources 47, p.180 (2022)
- 67Elabed et. al.: Sustainability of Medical Equipment in the Healthcare Industry: An Overview, p.3 (2019)
- 68Health Care Without Harm and Practice Greenhealth: Adressing Climate Change in the Health Care Setting, p.9. (n.d.)
- 69European Commission. Website:https://climate.ec.europa.eu/climate-change/consequences-climate-change_en (2023)
- 70Government of the Netherlands. Sustainable Healthcare. Website: https://www.government.nl/topics/sustainable-healthcare/more-sustainability-in-the-care-sector#:~:text=The%203rd%20Green%20Deal%20on,on%20climate%20and%20the%20environment. (2023)
- 71WHO guidance for climate-resilient and environmentally sustainable health care facilities. Geneva: World Health Organization; Licence: CC BY-NC-SA 3.0 IGO. (2020)
- 72Sherman, J. et.al. The Green Print: Advancement of Environmental Sustainability in Healthcare, Resources, Conservation and Recycling, Volume 161, 104882, ISSN 0921-3449, Doi: 10.1016/j.resconrec.2020.104882. (2020)
- 73Arab ul Mateen, Qasim Ali Nisar, Nadia Nasir, Fostering pro-environmental behaviors in the healthcare organizations: An empirical analysis of psychological and strategic factors, Asia Pacific Management Review, Volume 28, Issue 1, Pages 13-23, ISSN 1029-3132, Doi: 10.1016/j.apmrv.2022.01.004., (2023)
- 74Kruk, M. E., et. al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. The Lancet. Global health, 6(11), e1196–e1252. Doi: 10.1016/S2214-109X(18)30386-3(2018)
- 75Tomaselli, G., Garg, L., Gupta, V., Xuereb, P. A., & Buttigieg, S. C. Corporate Social Responsibility Application in the Healthcare Sector: A Bibliometric Analysis and Synthesis. International Journal of Information Systems and Social Change (IJISSC), 11(1), 11-23. Doi: 10.4018/IJISSC.2020010102 (2020)
- 76Sherman, J. D., MacNeill, A. J., Biddinger, P. D., Ergun, O., Salas, R. N., & Eckelman, M. J. Sustainable and resilient health care in the face of a changing climate. Annual Review of Public Health, 44, 255-277. (2023)
- 77Hu, H., Cohen, G., Sharma, B., Yin, H., & McConnell, R. Sustainability in Health Care. Annual Review of Environment and Resources, 47, 173-196.
- 78WHO. Background paper for the regional technical consultation on: Monitoring the Health-Related Sustainable Development Goals (SDGs) SEARO, New Delhi, India. https://cdn.who.int/media/docs/default-source/searo/hsd/hwf/01-monitoring-the-health-related-sdgs-background-paper.pdf?sfvrsn=3417607a_4&download=true (2017)
- 79Patil, A., Shardeo, V., Dwivedi, A., Madaan, J., & Varma, N. Barriers to sustainability in humanitarian medical supply chains. Sustainable Production and Consumption, 27, 1794-1807. (2021)
- 80Leite, H., Bateman, N., & Radnor, Z. Beyond the ostensible: an exploration of barriers to lean implementation and sustainability in healthcare. Production Planning & Control, 31(1), 1-18. (2020)
- 81Chate, A. B., Anikumar, E. N., & Sridharan, R. Analysis of barriers and enablers of sustainability implementation in healthcare centers. In Operations Management and Systems Engineering: Select Proceedings of CPIE 2019 (pp. 287-298). Springer Singapore. (2021)
- 82Leonidou, C. N., & Skarmeas, D. Gray shades of green: Causes and consequences of green skepticism. Journal of business ethics, 144, 401-415. (2017)
- 83Chiarini, A. and Vagnoni, E. (2016), “Environmental sustainability in European public healthcare: could it just be a matter of leadership?”, Leadership in Health Services, Vol. 29 No. 1, pp. 2-8. (2016)
- 84Evans, M. and Farrell, P. “A strategic framework managing challenges of integrating lean construction and integrated project delivery on construction megaprojects, towards global integrated delivery transformative initiatives in multinational organisations”, Journal of Engineering, Design and Technology, Vol. ahead-of-print. (2022)
- 85AlJaberi, O. A., Hussain, M., & Drake, P. R. A framework for measuring sustainability in healthcare systems. International journal of healthcare management. (2017)
- 86Dion, H., & Evans, M. Strategic frameworks for sustainability and corporate governance in healthcare facilities; approaches to energy-efficient hospital management. Benchmarking: An International Journal. (2023)
- 87Stevanovic, M., Allacker, K., & Vermeulen, S. Hospital building sustainability: The experience in using qualitative tools and steps towards the life cycle approach. Procedia environmental sciences, 38, 445-451. (2017)
- 88University of Vermont Medical Center. Website: https://www.uvmhealth.org/healthsource/sustainability-remains-a-priority-uvm-medical-center#:~:text=UVM%20Medical%20Center%20currently%20recycles,the%20hospital%20during%20the%20pandemic.
- 89University of Vermont Medical Center. Website: https://www.uvmhealth.org/healthsource/sustainability-remains-a-priority-uvm-medical-center#:~:text=UVM%20Medical%20Center%20currently%20recycles,the%20hospital%20during%20the%20pandemic.
- 90Cleveland Clinic Ohio. Website: https://my.clevelandclinic.org/about/community/sustainability/sustainability-global-citizenship
- 91Ärtzeblatt. Archiv. Nachhaltigkeit – Das grüne Krankenhaus. Website: https://www.aerzteblatt.de/archiv/147581/Nachhaltigkeit-Das-gruene-Krankenhaus (n.d.)
